- Therapeutic Cataract & Refractive
- Lens Technology
- Glasses
- Ptosis
- Comprehensive Eye Exams
- AMD
- COVID-19
- DME
- Ocular Surface Disease
- Optic Relief
- Geographic Atrophy
- Cornea
- Conjunctivitis
- LASIK
- Myopia
- Presbyopia
- Allergy
- Nutrition
- Pediatrics
- Retina
- Cataract
- Contact Lenses
- Lid and Lash
- Dry Eye
- Glaucoma
- Refractive Surgery
- Comanagement
- Blepharitis
- OCT
- Patient Care
- Diabetic Eye Disease
- Technology
Top 6 reasons to refer for cataract surgery
A referral of your patient to a cataract surgeon seems straightforward. You refer when the vision is subjectively affected by lens opacification. But thinking out of the box will enable you to help your patients in ways you may not consider.

A referral of your patient to a cataract surgeon seems straightforward. You refer when the vision is subjectively affected by lens opacification. But thinking out of the box will enable you to help your patients in ways you may not consider.
What are the most common reasons to refer a patient for lens replacement?
1. Visually significant cataract
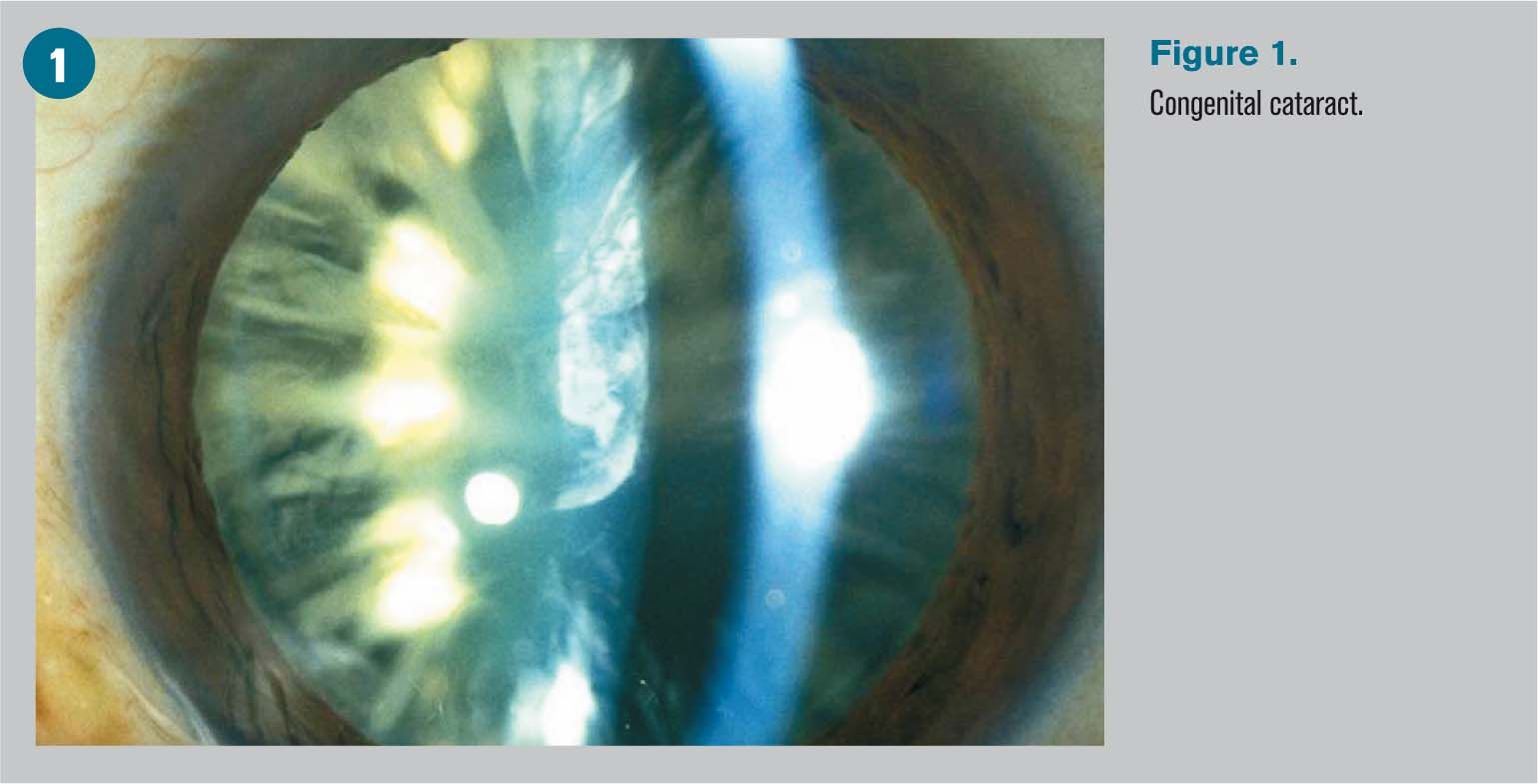
This is the obvious reason. When the clinical picture includes significant nuclear sclerosis, cortical and/or posterior subcapsular changes, and is associated with a reported significant loss of vision, refer. See Figure 1.
Related: An OD shares his perspective on his own cataract surgery

2. Myopic shift
Myopic shift is a reason to refer when it results in anisometropia. Nuclear sclerosis, as well as other types of cataracts, can result in a change of the index of refraction and a myopic shift.1,2 If the myopic shift is assymetrical, the refractive error may become significantly different. In some cases, it happens over six months, and the patient’s glasses become expensive and unwearable. Consider referring the patient with a detailed history of the change in manifest refractive and other subjective or objective signs.
Next: Narrow-angle glaucoma
3. Narrow-angle glaucoma
It is believed that removal of the crystalline lens creates more room in the anterior and posterior chambers and directly addresses narrow angle glaucoma. Several studies have reported significant drops in intraocular pressure (IOP) following phaco in cases of narrow angles.3,4 Phaco with IOL implantation vs. laser peripheral iridotomy was evaluated as treatment for acute primary angle closure by Husain et al.5 Researchers found less complications in the phaco treatment group and reported that phaco with IOL implantation resulted in a lower rate of defined IOP elevation at two years compared with laser peripheral iridotomy (LPI). However, the reduction in IOP was not found in all studies.6
More from Dr. Swartz: Put patients first with refractive surgery
4. Primary open-angle glaucoma
Even in cases of glaucoma with normal angles (POAG), the removal of the lens may reduce IOP. Mayer et al studied predictive factors for IOP reduction following phacoemulsification and found that at 12 months, pre-operative IOP and number of anti-glaucoma medications remained correlated with total IOP reduction following surgery. At 12 months, the IOP of the narrow-angle glaucoma and POAG groups were not significantly different.7

Bilak et al studied biometric parameters, including axial length, anterior chamber depth and lens thickness relative to IOP.8 They reported decreased axial length and IOP with increased anterior chamber depth one month after cataract surgery. They suggested the best parameter for estimation of postoperative IOP reduction was preoperative IOP. Patients with higher IOP tend to do enjoy the largest decrease in IOP following phaco.9
Next: Medical necessity
5. Medical necessity
This includes loss of visualization of the retina in cases of glaucoma or retinopathy, as well as limitation of mobility by vision reduction. While inactive patients may think their 20/50 vision is not hindering their sedentary lifestyles, their eyecare practitioners who need to assess their retinas for diabetic changes may feel differently. Also, cataractous reduction in contrast sensitivity increases the risk of a fall and affects stability. Cataract surgery has been reported to improve postural stability and decrease risk of falling.10

6. Dysfunctional lens syndrome

Dysfunctional lens syndrome (DLS) is a new term in the vision arena, typically used to describe patients who complain about their visual quality due to early changes in the lens. These patients often underwent elective vision correction for distance and present to your office reporting their “LASIK wore off.” While their lens changes may not warrant cataract surgery under the insurance guidelines, early to moderate lens changes may be the reason for their complaints. No spectacle or contact lens correction is going to make them happy.
Luckily, we now have technology to demonstrate the visual loss associated with DLS (Figure 2). Surgeons will consider a refractive lens extraction in these cases more than they may have 10 years ago. This option is, of course, not covered by insurance. Low risk of complications with phacoemulsification combined with improved visual outcomes make this choice more popular among those able to afford it. This is particularly true with the treatment of presbyopia with lens replacement, a possibility those who enjoyed the benefits of LASIK may feel comfortable considering as they age.
Do not assume your patients are not interested in surgical vision correction. If you give them options, you might be surprised at the choices your patient makes. And they will thank you.
References
1. Iribarren R, Iribarren G. Prevalence of myopic shifts among patients seeking cataract surgery. Medicina (B Aires). 2013;73(3):207-12.
2. Samarawickrama C, Wang JJ, Burlutsky G, Tan AG, Mitchell P. Nuclear cataract and myopic shift in refraction. Am J Ophthalmol. 2007 Sep;144(3):457-9.
3. Husain R1, Gazzard G, Aung T, Chen Y, Padmanabhan V, Oen FT, Seah SK, Hoh ST. Initial management of acute primary angle closure: a randomized trial comparing phacoemulsification with laser peripheral iridotomy. Ophthalmology. 2012 Nov;119(11):2274-81.
4. Brown RH, Zhong L, Lynch MG. Lens-based glaucoma surgery: using cataract surgery to reduce intraocular pressure. J Cataract Refract Surg. 2014 Aug;40(8):1255-62.
5. Husain R, Gazzard G, Aung T, Chen Y, Padmanabhan V, Oen FT, Seah SK, Hoh ST. Initial management of acute primary angle closure: a randomized trial comparing phacoemulsification with laser peripheral iridotomy. Ophthalmology. 2012 Nov;119(11):2274-81.
6. Shao T, Hong J, Xu J, Le Q, Wang J, Qian S. Anterior Chamber Angle Assessment by Anterior-segment Optical Coherence Tomography After Phacoemulsification With or Without Goniosynechialysis in Patients With Primary Angle Closure Glaucoma. J Glaucoma. 2015 Dec;24(9):647-55
7. Mayer C, Berguin C, Passarin O, Sharkawi E. Predictive Factors for Intraocular Pressure Reduction after Phacoemulsification in Swiss Patients. Klin Monbl Augenheilkd. 2015 Apr;232(4):409-413.
8. Bilak S, Simsek A, Capkin M, Guler M, Bilgin B. Biometric and Intraocular Pressure Change after Cataract Surgery. Optom Vis Sci. 2015 Apr;92(4):464-70.
9. Brown RH, Zhong L, Lynch MG. Lens-based glaucoma surgery: using cataract surgery to reduce intraocular pressure. J Cataract Refract Surg. 2014 Aug;40(8):1255-62.
10. Schwartz S, Segal O, Barkana Y, Schwesig R, Avni I, Morad Y. The effect of cataract surgery on postural control. Invest Ophthalmol Vis Sci. 2005 Mar;46(3):920-4.
