- Therapeutic Cataract & Refractive
- Lens Technology
- Glasses
- Ptosis
- AMD
- COVID-19
- DME
- Ocular Surface Disease
- Optic Relief
- Geographic Atrophy
- Cornea
- Conjunctivitis
- LASIK
- Myopia
- Presbyopia
- Allergy
- Nutrition
- Pediatrics
- Retina
- Cataract
- Contact Lenses
- Lid and Lash
- Dry Eye
- Glaucoma
- Refractive Surgery
- Comanagement
- Blepharitis
- OCT
- Patient Care
- Diabetic Eye Disease
- Technology
Minimize symptoms of dry eye disease in refractive surgery patients
Laser refractive procedures such as laser-assisted in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK) are considered some of the most ground-breaking inventions in elective eye surgery.
As a post-PRK patient and OD who manages pre- and postop visits for a large OD/MD practice specializing in refractive surgery, I have seen firsthand the benefits of being able to wake up on any given day and just see.
Preoperative
I have found that the best way to combat postoperative dry eye is to know about it pre-operatively. Many patients seek refractive surgery due to the inability to tolerate contact lenses, and it is thought that the prevalence of patients already suffering from dry eye symptoms prior to refractive surgery ranges from 38 percent to 75 percent of patients.1
Taking the time to explain to each patient exactly why it is necessary that their corneas be “primed and prepped” before surgery is an important step in the pre-op process. Forgoing aggressive treatment of dry eye disease (DED) and ocular surface irregularities may cause surgery to be delayed, or worse, the end results may not be as precise as they could have been.
Although there is no way to predict post-refractive dryness for an individual patient, pre-existing dry eye disease is a known risk factor for ocular surface problems after refractive surgery.2
Postoperatively, up to 95 percent of patients experience symptoms of dry eye at some point over the first three months after surgery, which often improves with time.2
The quicker optometric physicians can identify the cause of a patient’s subjective complaints, the faster patient satisfaction can be improved and the need for surgical enhancements minimized.
Before referring a patient for surgery or a refractive enhancement, ask: Has everything been done in order to solve the all ocular surface concerns?
To help triage a post-refractive surgery patient who is seeing well-but who may be symptomatic with “blur,” “glare,” or “halos”-assess the following before referring for an enhancement.
Related: diving into dry eye can help physicians solve patients' woes
Eyelid and tear function
Eyecare providers can dive deeper into investigating symptoms of DED by first looking at the eyelid function. Assessing the eyelid margins and blink status, as well as investigating the meibomian gland (MG) function and tear quality, can help to grasp the severity of DED.
In patients having trouble with dry eye symptoms, observing the eyelids often reveals incomplete blinks and/or MG dysfunction and dropout. Spending a few extra minutes with these patients to help educate them about their dry eye condition has shown to be beneficial to patients and their overall satisfaction with surgical outcomes.
For symptomatic post-refractive dry eye patients, I often recommend preservative-free artificial tear lubrication such as Refresh Mega-3 (Allergan), which fortifies the lipid layer and helps to prevent tear evaporation.
Systane Complete (Alcon) is another option known for its nano-droplet technology, which may help target all three layers of the tear film to hydrate and add tear evaporation protection.
Other options to improve MG function include TearCare (Sight Sciences) and LipiFlow (Johnson & Johnson Vision)-devices that apply heat to the meibomian glands so the glands can be more easily expressed, thus helping to increase tear break-up time (TBUT) and reduce dry eye symptoms.1
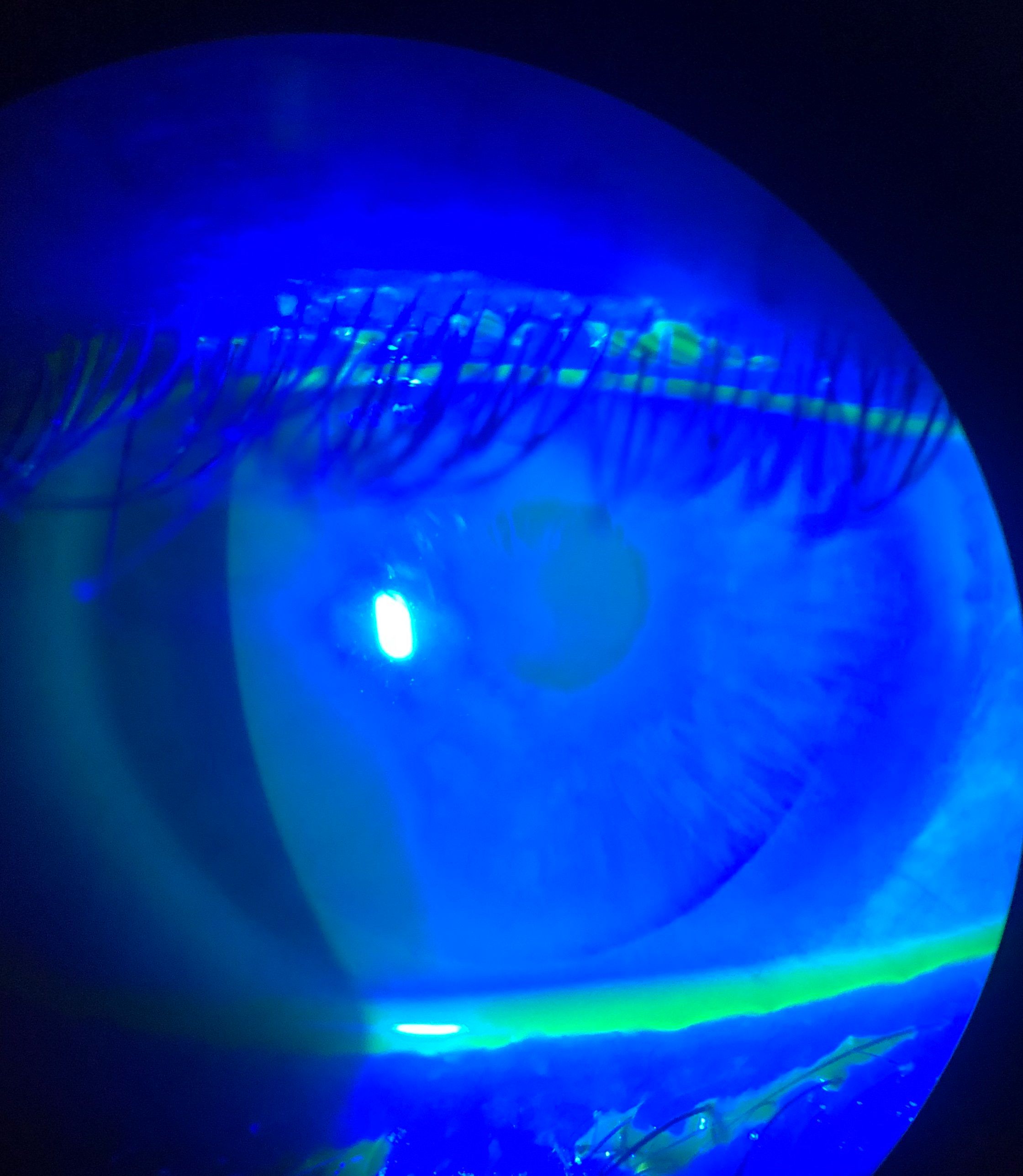
Inferior corneal staining
I often see post-refractive patients also affected by common environmental factors that cause intermittent blur, glare, and symptoms of DED.
Whether due to a continuous positive airway pressure (CPAP) machine, living in a high-altitude area with low humidity, extended computer use, riding in an arid airplane, poorly placed vents at home/work-all of which cause dry eyes-it is important to identify and treat these likely culprits of chronic environmental dryness.
In addition to artificial tears, punctal plugs can also be inserted bilaterally to delay tear drainage and improve the amount of time tears stay on the ocular surface.
Other dry eye treatment for post-refractive surgery patients include Xiidra (lifitegrast, Novartis) to improve DED signs and symptoms and Restasis (cyclosporin, Allergan), an immunomodulator to help increase tear production. Note that Cequa (cyclosporin, Sun Pharma) is hitting the market as well.
Related: Managing dry eye key to patient satisfaction after cataract, refractive surgeries
Pupil size
A patient with a larger pupil size can experience increased higher-order aberrations; thus, an increase in the blur and glare symptoms observed by the patient. Large pupils paired with ocular surface irregularities can have an even greater influence on the overall quality of vision perceived by the patient.
To help minimize this glare, I recommend OTC Lumify (brimonidine tartrate ophthalmic solution 0.025%, Bausch + Lomb) for its secondary off-label effect of diluted brimonidine. Just like other selective alpha-2 agonists, Lumify reduces redness by constricting the conjunctival venules (instead of arterioles like tetrahydrozoline, Visine). The use of brimonidine has been shown in office to have a small, yet often symptomatically positive effect on pupil size in scotopic conditions, which seems to help decrease the glare and halo effects of night driving. 4
Wrapping up
To most effectively maximize results and minimize enhancements rates, treating any hint of dryness before surgery helps “prime and prep” the cornea for the best visual and surgical outcome.
Dry eyes can significantly affect patients’ perception of their surgical outcomes and level of satisfaction; therefore, continuing to treat DED before and after refractive surgery sets up the patient for success.
Whether choosing artificial tears, punctal plugs, TearCare, LipiFlow, Xiidra, or Restasis to treat DED in post-refractive surgery patients, the root of the dryness should be established and discussed with the patient early in the process.
By making the patient aware of any dry eye and ocular surface problems-and taking the time to explain the realistic expectations of possible dry eyes in the future-it is easier for the patient to understand how to easily combat intermittent symptoms.
Assessing the overall eyelid and tear function, inferior corneal staining, and pupil size as factors that could be playing a role in overall quality of vision after surgery can help tailor a dry eye treatment regimen.
Prior to referring for LASIK/PRK or a refractive enhancement, it is ideal to identify and aggressively treat underlying dry eye and OSD.
Disclosures:
References
1. Cohen E, Spierer O. Dry Eye Post-Laser-Assisted In Situ Keratomileusis: Major Review and Latest Updates. J Ophthalmol. 2018 Jan 28;2018:4903831.
2. Yu EY, Leung A, Rao S, Lam DS. Effect of laser in situ keratomileusis on tear stability. Ophthalmology. 2000 Dec;107(12):2131-5.
3. Solomon R, Donnenfeld ED, Perry HD. The effects of LASIK on the ocular surface. Ocul Surf. 2004 Jan;2(1):34-44.
4. Edwards JD, Burka JM, Bower KS. Effect of brimonidine tartrate 0.15% on night-vision difficulty and contrast testing after refractive surgery. 2008 Sep;34(9):1538-41.
