Blog: How to manage refractive surgery surprises
The views expressed here belong to the author. They do not necessarily represent the views of Optometry Times or UBM.
It is never a good sign when a technician says a patient is not happy when exiting the exam lane. I do not like to go in these rooms. Having worked in the refractive surgery world, I know how to calm most patients down.
In most cases, the surgery did not meet the patient’s expectations.
Reasons for this include:
• Post-operative pain
• Blurry vision
• Dry eyes
• Increased ocular surface disease
• Patients saying, “It was expensive, “My result was not perfect” and “I can’t read”
In this case, my patient was returning one week after his cataract surgery, and he had undergone LASIK 15 years ago. My patient reported he could read. Because distance vision was the goal, he was upset. The patient’s previous LASIK complicated his intraocular lens (IOL) calculations.
At one week after the second eye, he was 20/20 at near and computer but unable to see far away.
Surgeons strive to minimize postoperative refractive errors using modern biometry, and some patients pay extra for intraoperative aberrometry to reduce the risk of residual refractive error.
Patients with a history of refractive surgery are more likely to suffer from residual refractive error after cataract surgery.
Here are nine reasons patients may not receive the optimum IOL power.
1. Poor ocular surface affecting corneal measurement
Corneal curvature is required for IOL calculations. Unstable tear film, keratitis, dry eye, and epithelial basement membrane dystrophy (EBMD) are common causes of unstable and- therefore-erroneous corneal curvature measurements.
Ocular surface disease should be addressed prior to referral for cataract surgery.
2. Contact lens wear was not discontinued for enough time
If the cornea does not return to its natural shape prior to measurement, the corneal power will be inaccurate.
Note that contact lenses must be removed prior to measurement and not the actual surgery day because the corneal power measurement is typically performed prior to surgery.
Gas permeable contact lens patients should wear glasses for several weeks prior to measurement for best results. Repeated keratometry and/or topography measurements should be stable prior to being referred for IOL measurement testing.
3. Corneal measurements performed after cornea was touched with Goldmann tonometer
Goldmann tonometry changes the corneal power. All IOL measurements should be performed prior to administering drops or touching the cornea. See Table 1.
4. Extremely short or long axial lengths results in calculation errors
The average axial length is 23.30 mm. Errors may occur using IOL calculation formulas in short eyes (<22 mm) and long eyes (>25 mm).
Axial length errors are amplified in short eyes. Posterior staphyloma results in elongated axial lengths, leading to postoperative hyperopia. See Table 1.
5. Shallow or deep anterior chambers are directly related to effective lens position (ELP)
ELP is the distance of the principal plane of the IOL from the cornea. A deep chamber in a hyperope will introduce error into the measurements. See Table 1.
6. Keratorefractive surgery (KRS, such as radial keratotomy, Lasik, or PRK) results in reduced precision of corneal power measurement
Biometry for IOL calculations assumes the natural spherical curvature of the cornea, which is directly altered by KRS.
Changing the central cornea shape, and possibly the posterior corneal curvature, alters this math. Most of our vision occurs within the central effective zone, which many devices do not measure.
The greater the amount of excimer treatment (and greater the change in corneal curvature), the greater than error.
Theoretically, myopic treatments require an increase in IOL power. Hyperopic treatments require a decrease in IOL power. RK incisions typically cause a hyperopic result, increasing with the amount of incisions.1 See Table 1.
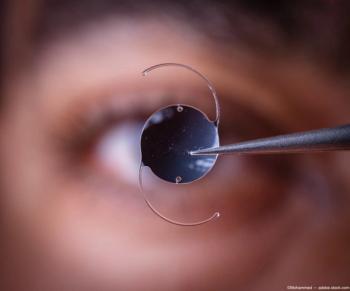
6. The IOL is inserted upside down
Inadvertent insertion of a posterior chamber intraocular lens with a reversed front to back orientation will result in residual refractive error in a single-piece IOL.
7. Unpredictability of final effective lens position
ELP in the original IOL calculation formulae was a constant because most implants were anterior chamber lenses.
Posterior chamber lenses sit farther back, introducing more error into the calculations.
8. Even in a perfect situation, there are limitations to the precision and accuracy of biometric measurement
This testing is typically performed by technicians, who may not be detailed-oriented. The tests are performed on living, breathing patients in a clinical environment that is often busy.
9. Post-operative movement
Anterior movement of the lens implant may occur due to capsular bag fibrosis and contraction. Toric lenses may also rotate.
Residual refraction
What do you do when there is a significant residual refraction? Rule number one: refractive error is not pathological.
While being blurry is annoying, it is not a medical problem. Patients should be reassured that the surgery went fine and the math involved is the only problem. Math problems can be solved.
Remeasure corneal curvature, autorefraction, manifest refraction, and aberrometry. Also dilate to examine the IOL.
I prefer to use other methods to evaluate the residual refraction to better understand what needs to be changed.
Look for misplaced optics, which may indicate a reversed implant or an implant in the sulcus rather than the capsular bag. Evaluate toric lenses for axis positioning and determine if the IOL has moved from its planned axis.
When the patient is mistakenly nearsighted, I routinely point out the advantages to having near vision before taking it away. The patient in the case mentioned earlier was -1.50-0.75 x 180 (20/20) OD, and -1.25-0.75 x 180 (20/20) OS.
He could read and use computers comfortably. I corrected him with contact lenses and showed him the effect of corrected distance vision on functioning at near.
His complaint when he returned a week later? “I can’t read.”
Surgery post-cataract surgery
Refractive correction after cataract surgery can be addressed using spectacles, contact lenses, refractive surgery, IOL exchange, or a piggyback IOL.
For patients who were not hoping for spectacle-free distance vision, wearing spectacles may not be a significant problem. problem. However, anisometropia may complicate spectacle correction. Wearing contact lenses works well if anterior segment health allows.
Refractive surgery post-cataract surgery can be successfully performed. PRK is preferred to avoid LASIK induced dry eye. PRK may be preferred to avoid LASIK-induced dry eye, so when discussing excimer surgery, do not speak of LASIK specifically. Leave options open for the surgeon.
It is best to wait three months after cataract surgery for refractive surgery to ensure the refraction is stable and corneal incisions have healed.
IOL exchange
A lens may be removed and exchanged for another-hopefully more correct-IOL. IOL exchange cannot be performed after a YAG laser capsulotomy, so be sure you are happy with the IOL prior to performing the procedure.
This may be the better option when refractive errors-particularly anisometropia- are large, requiring significant change in refractive corneal power. This may also be preferred by surgeons who do not perform KRS.
Lens exchanges should occur quickly, prior to development of lens capsule fibrosis. Piggybacking involves the implantation of a second lens in the posterior chamber in front of the original IOL in the capsular bag. It is easier and safer than removing the lens.2
I always demonstrate the intended outcome using loose lenses or contact lenses prior to surgery to ensure the patient’s full understanding of the refractive target.
Reduce effect of residual refractive error
The best way for optometrists to reduce the effect of residual refractive error is to:
• Tell all patients you refer for cataract surgery that there is a risk they may need glasses full-time after surgery.
• Mention the increased risk before surgery in all patient with a history of any keratorefractive surgery.
• Mention the risk before surgery again because the first time, the patient probably did not hear you.
• If the patient is unhappy following cataract surgery, calmly assess a situation by remeasuring the numbers, and reassure the patient.
• Blame the math. Everyone hates math anyway.
References:
1. Ladi JS. Prevention and correction of residual refractive errors after cataract surgery. J Clin Ophthalmol Res. 2017;5:45-50.
2. Amon M, Kahraman G. Enhancement of refractive results after intraocular lens implantation. European Ophthalmic Review. 2011,5(1):59-61.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.