Don’t overlook blepharoptosis in clinical practice
Noninvasive treatments can help patients with ptosis improve their visual field.
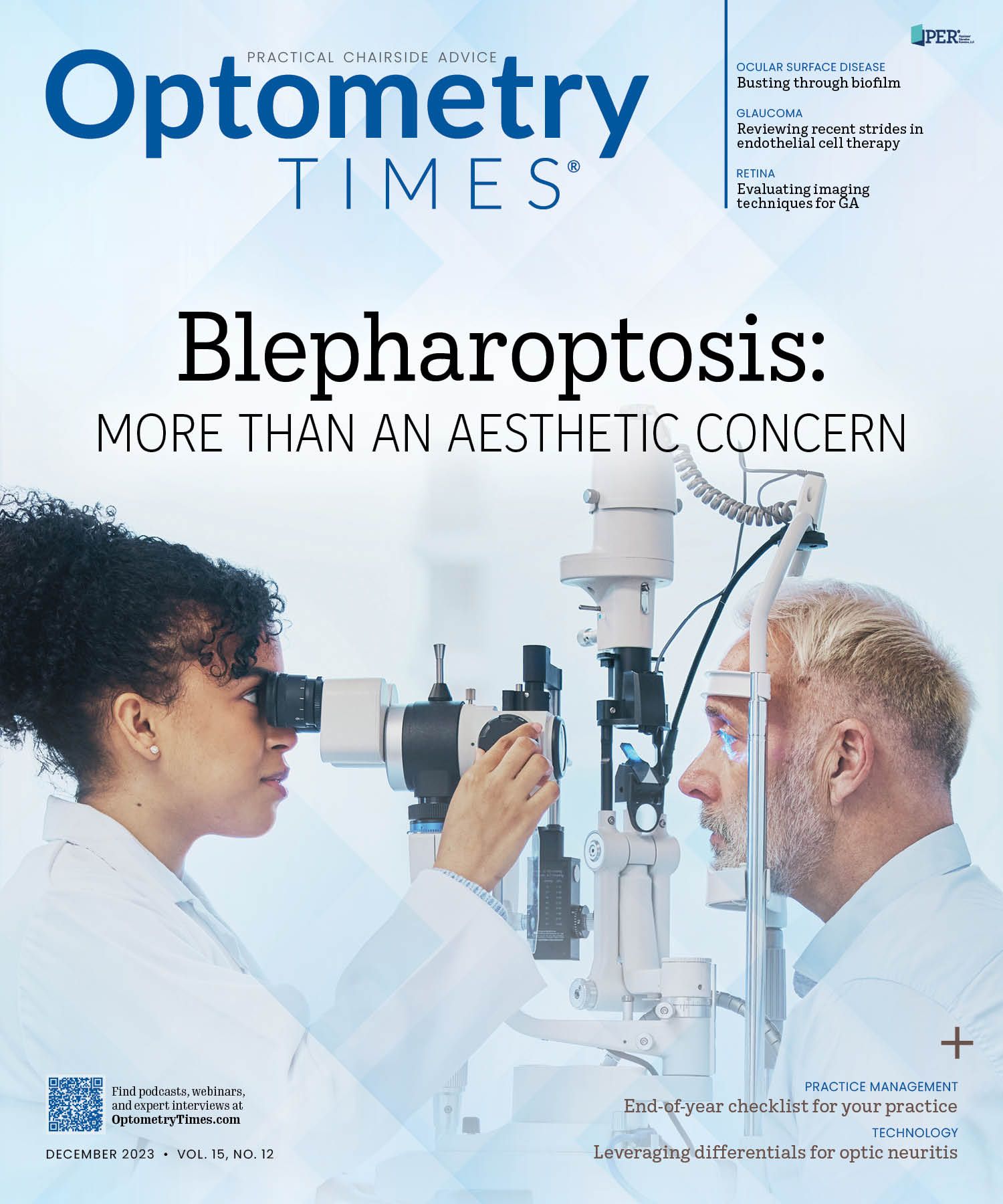
Image credit: Adobe Stock / Clement C/peopleimages.com

Blepharoptosis is a common eyelid disorder that can cause significant visual impairment,1 but the issue has long been overlooked in clinical practice because, other than surgery, optometrists were unable to offer much help.
With surgery being the primary option, most patients opted out. However, as noninvasive treatments—from mechanical aids to daily eye drops—reach the pipeline and market, optometrists are realizing a meaningful opportunity to improve quality of life for these patients.
Many health conditions can lead to acquired ptosis, including tumors, vascular issues, and third cranial nerve palsy, but the most common cause is a gradual, age-related change in eyelid tonicity.
Because ptosis had not historically been a focus in our practice, I wasn’t aware of how acutely it was compromising vision for my patients. Although they tried to describe the problem, most patients could only tell us that something had changed in their vision.
The conversation shifted when I started noticing a trend in my retinal imaging of these patients: Their low-lying upper lids and/or eyelashes were casting a shadow that obscured our view of the inferior fundus image. It occurred to me that if we couldn’t fully visualize patients’ retinal images, they were probably experiencing a reduced field of vision.
To address that problem, I began prescribing an eye drop approved for the treatment of acquired ptosis, and my patients immediately appreciated a difference in their perception of light, describing their vision as brighter, fuller, or sharper.
Based on my experience, I feel it is incumbent on optometrists to pay close attention to the signs and symptoms of ptosis so we can intervene when necessary. We should not only be cognizant of the eyes but also of the eyelid position during every examination, as this is the best way to ensure this burdensome condition is appropriately managed.
Studying a topical treatment
The drop offered in our office is oxymetazoline hydrochloride ophthalmic solution 0.1% (Upneeq; RVL Pharmaceuticals plc), a once-daily treatment approved by the FDA based on phase 3 evidence that it safely and effectively improves superior visual field and eyelid lift in patients with acquired ptosis.2 The medication works by stimulatingα-adrenergic receptors on Müller muscle, activating the muscle and raising the eyelid margin. It has a 5 to 1 preference for the α-1 vs α-2 receptors.
I began prescribing oxymetazoline 0.1% shortly after its approval in July 2020, and started to see the improvements in visual function and began to understand its utility in improving our patients’ visual fields.
I illustrated that experience in a poster demonstrating that retinal scanning is an effective way to identify and track the progression of acquired ptosis, as well as the condition’s response to topical treatment.3
The study, titled “Use of Confocal Scanning Retinal Imaging to Identify Visual Field Limitations and Evaluate Effects of Oxymetazoline Hydrochloride Ophthalmic Solution 0.1% Treatment in Adult Patients With Acquired Ptosis,” was presented at the 2023 Southeastern Educational Conference of Optometry International.
Of 5 participants, 1 was followed for ptosis progression with confocal scanning retinal imaging (CSRI). The other 4 participants were evaluated for ptosis, with CSRI administered at baseline and then again 15 to 30 minutes later, after treatment with oxymetazoline 0.1%.
Followed for progression was a 70-year-old woman with an ocular history of epiretinal membrane (ERM) in her left eye and mild bilateral cataracts who presented with mild, age-related ptosis in her right eye. At a 6-month follow-up for ERM and cataracts, the inferior portion of her retinal image was more obscured on CSRI, demonstrating ptosis progression that was causing superior visual field limitation (Figure 1).
The 4 additional patients presented with obscured views inferiorly on retinal imaging that significantly diminished after they received treatment with 1 drop of oxymetazoline 0.1% in each of their affected eyes. Those patients included the following:
- A 43-year-old woman with myopia who had switched from rigid gas permeable lenses to soft lenses and had mild ptosis (Figure 2).
- A 78-year-old woman with bilateral pseudophakia and mild ptosis (Figure 3).
- A 49-year-old man with bilateral myopia, presbyopia, and astigmatism who had moderate ptosis (Figure 4).
- A 51-year-old woman with bilateral myopia, presbyopia, and astigmatism who had severe ptosis (Figure 5).
I grade ptosis severity based on how much of the superior portion of the iris is occluded by the upper eyelid. In a normal patient, the upper lid margin sits at the margin of the upper visible iris diameter. In mild ptosis, the lid obstructs a portion of the top 50% of the iris between the superior pupil and superior margin of the iris diameter. A patient is graded as having moderate ptosis if the lid margin lies between the superior pupil margin and below the halfway point to the superior iris margin. Finally, an upper eyelid margin that covers any portion of the pupil constitutes severe ptosis. Clinically, this seems to be a simple and efficient way to grade lid position. We scanned the retina using EIDON TrueColor Confocal technology, providing high-resolution, widefield color images.
Our conclusion was that CSRI is a viable, objective tool for assessing the effect of ptosis on the light entering the eye and the immediate effects after a topical treatment.
Furthermore, we found that a reduction in inferior image obstruction was visible in images as soon as 15 minutes after administration of oxymetazoline 0.1%, providing further evidence that the medication effectively treats ptosis.
Treating ptosis noninvasively
Oxymetazoline 0.1% is among a host of topical drops, including apraclonidine, that have been studied as potential treatments for ptosis.4 Although all these topical drops work by causing Müller muscle to contract, oxymetazoline 0.1% is the only one approved by the FDA. Patients can use the medication monocularly to improve asymmetries in their visual function, or they can administer it in both eyes daily or as needed to improve vision before activities such as driving.
Within the ptosis population, oxymetazoline 0.1% has its most pronounced effect in patients with very little fat in the upper lid tissue. These patients often have eyelids that lie against the globe, so any elevation in the lid margin is easily seen. The treatment effect is less pronounced in patients with dermatochalasis.5 Although the lid will still lift if they have concurrent ptosis, the excessive skin may mask some of the lid margin elevation, making it less obvious.
In addition to oxymetazoline 0.1%, there are mechanical aids that can help raise the upper eyelid. A key option is scleral lenses, which provide a unique opportunity for patients requiring specialty lenses to help their ptosis. Because of the way they fit, these lenses vault the cornea, creating a ledge over which the eyelid must blink. This tends to hold the lid up, providing a more normalized lid position for patients with ptosis.
Strengthening our practice
Although options for treatment have previously been limited to surgical procedures, pharmaceutical approaches have made the management of ptosis more accessible in clinical practice. The ability to work with patients to improve not only their appearance but also their visual function is providing eye care practitioners with a more holistic approach for the treatment of blepharoptosis. By routinely diagnosing and treating this once overlooked condition, we can help countless patients improve their quality of life.
References
1. Bacharach J, Lee WW, Harrison AR, Freddo TF. A review of acquired blepharoptosis: prevalence, diagnosis, and current treatment options. Eye (Lond). 2021;35(9):2468-2481. doi:10.1038/s41433-021-01547-5
2. FDA approves Upneeq. Drugs.com. July 9, 2020. Accessed October 2, 2023. https://tinyurl.com/8fr9trf9
3. Brujic M. SECO 2023: incorporating confocal scanning laser imaging in practice. Optometry Times. March 5, 2023. Accessed October 4, 2023. https://www.optometrytimes.com/view/seco-2023-incorporating-confocal-scanning-laser-imaging-in-practice
4. Karpecki PM. Noninvasive ptosis management. Review of Optometry. June 15, 2020. Accessed October 3, 2023. https://reviewofoptometry.com/article/noninvasive-ptosis-management
5. What impact can droopy eyelids have on vision? Healthline. Reviewed November 10, 2021. Accessed October 3, 2023. https://www.healthline.com/health/eyelid-disorders/what-impact-can-droopy-eyelids-have-on-vision