- March digital edition 2021
- Volume 13
- Issue 3
How to prevent infection after LASIK or PRK
Have a plan when infection occurs
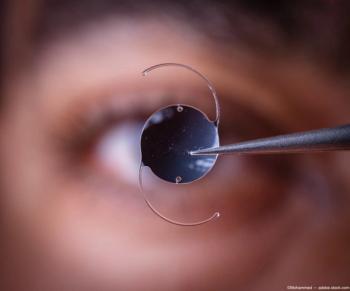
I RELAY THE RISKS of laser vision correction surgery to all my patients in the same way. I cover dangers inherent in any surgical procedure, such as those involving anesthesia, bleeding, and infection. Fortunately, laser vision correction does not require general anesthesia and the cornea does not have blood vessels (at least it should not). Therefore, the only risk ODs want to prevent is infection. This article covers the risks of infection, how to minimize them, and what to do if a patient has or is suspected of having a corneal infection post laser vision correction.
Risk of infection
The risk of infection following a laser vision correction procedure has been well studied and is rare. In a retrospective review of 204,586 cases, the incidence of all infections was 0.035% for laser-assisted in situ keratomileusis (LASIK).1 Also, a survey of 56 LASIK surgeons from the American Society of Cataract and Refractive Surgery (ASCRS) reported 116 cases of post-LASIK microbial keratitis out of an estimated 338,550 procedures, representing an infection rate of 0.034%2
In a separate review of 18,651 cases, the incidence of all infections was 0.21% for photorefractive keratectomy (PRK).3 A smaller study of 4492 eyes yielded an infection rate of 0.2% for PRK.4 Although the risk of keratoectasia is less when undergoing PRK, it appears the risk of infection is significantly greater. It is believed this is because the 6 to 8 mm epithelial defect created during PRK versus the flap edge in LASIK.
Staphylococcus aureus is the most common pathogen for bacterial keratitis in general, and it is the most common infectious agent post laser vision correction.5,6 Prior to the introduction of fourth-generation fluroquinolones, atypical mycobacteria such as Nocardia were the next most common pathogen. Currently, there is an increase in methicillin-resistant Staphylococcus aureus (MRSA) infections. It is believed that LASIK and PRK infections comes from the normal flora of a patient’s lids and lashes during surgery or immediately after surgery. The patient’s signs and symptoms usually present in the first week after surgery.
Nonactive herpetic infections are not an absolute contraindication for laser vision correction; therefore, there are cases of re-activation of the virus after PRK and LASIK. In case reports from the literature, none of these infected patients were pretreated with anti-viral medication.7 Currently, many surgeons will pre-treat patients with known viral infections with acyclovir or similar antivirals for up to 1 month prior to surgery and 1 month after surgery.
Prevention
Prevention of postoperative infections begins at the preoperative visit. Active blepharitis and ocular surface disease are conditions that increase the risk of post-operative infection.8 Careful examination of the tear layer, ocular surface, and lids and lashes must be a critical part of every patient’s preoperative evaluation. Each condition should be treated appropriately prior to surgery. Because health care workers are often MRSA carriers, it is important to know the patient’s occupation; those patients should be treated differently both intra and postoperatively to reduce the risk of MRSA infection.
Prophylaxis for ocular infection usually begins with a thorough cleaning of the lids and lashes with a povidone-iodine (Betadine; Alcon) scrub. Of 4 widely used antiseptics (povidone-iodine, polihexanide, chlorhexidine and octenidine), povidone-iodine has a broad spectrum of antimicrobial activity that includes gram-positive and gram-negative bacteria, bacterial spores, fungi, protozoa, and viruses.
Intra-operatively, many surgeons use a drop of fourth-generation fluroquinolone prior to making the LASIK flap and at the end of the procedure. Typical anti-infective postoperative treatment for LASIK is 1 drop every 4 hours while awake for the first week after surgery. For known MRSA carriers, mupirocin (Bactroban; GlaxoSmithKline) ointment is used preoperatively and polymyxin B sulfate and trimethoprim (Polytrim; Allergan) drops are added to the postoperative regime.
Symptoms
Patient symptoms for infection post laser vision correction are similar to those of general microbial keratitis; pain, photophobia, and reduced vision. These symptoms can present as early as the first postoperative day and rarely do they occur after the first week. Slit-lamp evaluation should differentiate between superficial punctate keratitis (SPK), which is common on the first post-operative day, versus corneal infiltrates, which are uncommon.
White infiltrates should be further differentiated between those within the flap margin and those outside of the flap. There is a much greater concern for those infiltrates within the flap margin. Our clinic has always taken a conservative approach and treated those infiltrates within the flap margin as MRSA even in the absence of an epithelial defect and prior to culture.
Postoperative care
If a postoperative infection is suspected, a change in protocol is often most effective. Additionally, it is important to inform the operating surgeon and generally referred to the operating surgeon. Having the operating surgeon’s contact information is critical in timely communication regarding patients with infections. It is typical to alternate the fourth-generation fluroquinolone with fortified cefazolin 50 mg/ml every 30 minutes.
If MRSA is suspected, vancomycin is recommended as a substitute for cephazolin. The patient should be seen daily until the condition improves. Vancomycin ophthalmic preparation needs to be stored frozen or prepared by a compounding pharmacy; therefore, it is best to have a plan before encountering a MRSA infection. Post-operative infections can advance rapidly, making this condition the most emergent that one would likely encounter in laser vision correction.
Laser vision correction is a safe and effective procedure. As with any surgical procedure, there comes some risk. Fortunately, the risk of infection is low. Carefully screening patients, treating pre-operative conditions, and providing diligent post-operative care allow for even better surgical outcomes. Most importantly, having a plan for when an infection may occur greatly improves the odds of success.
References
1. Llovet F, de Rojas V, Interlandi E, et al. Infectious keratitis in 204 586 LASIK procedures. Ophthalmology. 2010 Feb;117(2):232-8. e1-4. doi: 10.1016/j.ophtha.2009.07.011
2. Donnenfeld ED, Kim T, Holland EJ, et al; American Society of Cataract and Refractive Surgery Cornea Clinical Committee. ASCRS White Paper: Management of infectious keratitis following laser in situ keratomileusis. J Cataract Refract Surg. 2005 Oct;31(10):2008-11. doi: 10.1016/j.jcrs.2005.10.030
3. de Rojas V, Llovet F, Martínez M, et al. Infectious keratitis in 18,651 laser surface ablation procedures. J Cataract Refract Surg. 2011 Oct;37(10):1822-31. doi: 10.1016/j.jcrs.2011.04.037
4. de Oliveira GC, Solari HP, Ciola FB, et al. Corneal infiltrates after excimer laser photorefractive keratectomy and LASIK. J Refract Surg. 2006;22(2):159-165.
5. Lakhundi S, Siddiqui R, Khan NA. Pathogenesis of microbial keratitis. Microb Pathog. 2017 Mar;104:97-109. doi: 10.1016/j. micpath.2016.12.013
6. Garg P, Chaurasia S, Vaddavalli PK, et al. Microbial keratitis after LASIK. J Refract Surg. 2010 Mar;26(3):209-16. doi: 10.3928/1081597X-20100224-07
7. Lu CK, Chen KH, Lee SM, Hsu WM, Lai JY, Li YS. Herpes simplex keratitis following excimer laser application. J Refract Surg. 2006 May;22(5):509-11.
8. Gimbel H, Anderson-Penno E. Laser Complications: Prevention and Management. Slack, Inc.; 1999.
Articles in this issue
almost 5 years ago
Vision rehabilitation of patients with traumatic brain injuryalmost 5 years ago
Multifocal lenses for presbyopia in eyes with previous corneal surgeryalmost 5 years ago
Know risks and benefits of ocular steroid usealmost 5 years ago
How to address dry eye in the challenging corneaalmost 5 years ago
New data in anterior segment laser surgeryalmost 5 years ago
Know 4 types of allergic eye diseasealmost 5 years ago
New therapy addresses dry eye flaresalmost 5 years ago
COVID-19 & migraine: Patient impact & management tipsalmost 5 years ago
Quiz: New data in anterior segment laser surgeryalmost 5 years ago
Think beyond anti-VEGF injectionsNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.