Turning inexperience into expertise in fitting scleral lenses
Building confidence and knowledge can reduce office visits and increase results.
Image Credit: AdobeStock/LoLoStock
Scleral lenses demand expertise. We can cause real harm by placing a hard piece of plastic on soft tissue. Although they require time to fit and are difficult to troubleshoot when problems arise, scleral lenses are life-changing for our patients.
We all want our patients to experience complication-free, comfortable wear with excellent vision. What we as an industry do not want are patients who turn away from this lens modality because of price, complications, or the feeling that scleral fitters do not know how to make the lenses successful. Unfortunately, unsuccessful situations can arise when a practitioner is inexperienced in the art and science of fitting scleral lenses.
A quick review of social media posts shows that there is a lot of uncertainty among doctors about the details of fitting scleral lenses. As an industry, we need to do a better job becoming expert scleral lens fitters.
Are all optometrists capable of becoming experts in scleral lenses? We believe so. Getting this right takes sacrifice, dedication, training, investment in the right equipment, and experience. If you have the interest, passion, and dedication, here is what it will take to hone your skills.
Training
Figure 1. Inadequate vault over the limbus leads to redness, discomfort, and refractive changes. This can easily be eliminated with proper training and equipment. (Image courtesy of Jeffrey Sonsino, OD, FAAO)

Chances are good that none of us learned to be an expert at fitting specialty lenses in optometry school. If you graduated from optometry school recently, you likely saw approximately 13 scleral lens patients in the school’s clinic and 44 in external rotations by the time you graduated.1 If you graduated before 2006, there was no scleral lens training at all, because the lenses were not widely available yet (Figure 1).
Completing residency training in specialty contact lenses is one way to quickly arrive at a basic level of competence, but at the time of this writing, there are only 25 accredited cornea and contact lens residency programs in the US, Puerto Rico, and Canada combined.2 That is hardly sufficient to satisfy the demand for specialty contact lenses in America.
For the majority of us, additional training is needed after completing optometry school or residency. Most laboratories offer some type of course for practitioners interested in fitting their specific lens design. Continuing education programs are available for scleral training at most meetings nowadays. Organizations such as the Scleral Lens Education Society and the Gas Permeable Lens Institute offer free, nonbranded
training lectures each month taught by top practitioners in the field. These organizations exist to make us all better clinicians.3
To gain expertise and be successful, practitioners need to learn basic scleral lens fitting techniques, proper placement of lenses on eyes and evaluation of those fits, how to do advanced troubleshooting, and all the details of billing and coding. In addition, they need to practice on patients with the diseases that can be treated with scleral lenses.
The Scleral Consultative Institute (SCI), which is funded by gas permeable (GP) laboratories and button manufacturers,4 provides no-cost training to practitioners who want to learn excellence in scleral lens fitting.5 Practitioners experience the industry’s most comprehensive scleral lens experience. It takes place in an optometry office setting, so participants can translate what is learned directly into practice. An entire afternoon is spent on billing vision and medical insurance for medically necessary contact lenses. Interested practitioners can contact their laboratory to apply for sponsorships to attend the events.
Equipment
Once a practitioner has the requisite training, several devices aid in evaluating and managing the scleral lens process as well as the underlying diseases.
Corneal topography
Although corneal topography cannot be used to select diagnostic lenses, it is crucial for proper diagnosis and monitoring of a patient’s corneal disease state. If you are seeing patients who use scleral lenses, then you must also monitor the underlying condition. In fact, payers often demand monitoring of the underlying condition to build the reimbursement structure.
Figure 2A
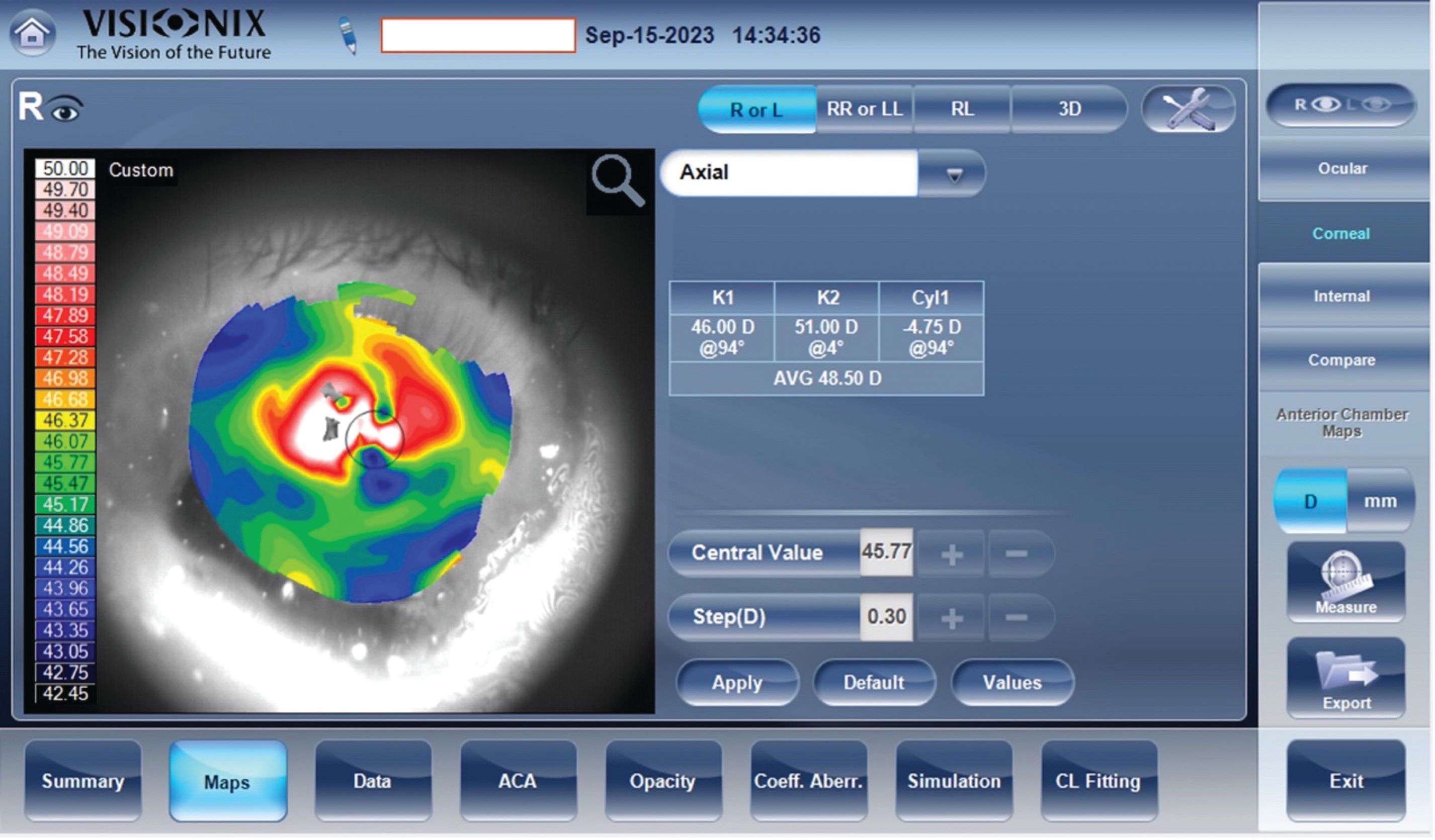
Figure 2B. Corneal topography of a highly irregular cornea. This patient was involved in a laboratory explosion when he was a graduate student in chemistry. The mortar and pestle exploded and embedded thousands of shards of porcelain into his cornea and conjunctiva, many of which remain 40 years later. A scleral lens was fit to improve his vision from 20/100 to 20/50. (Images courtesy of Jeffrey Sonsino, OD, FAAO)

There are other uses for corneal topography as well. Overtopography (taking a topographical map above a scleral lens) can assess the tear film quality and measure centration of a lens over the visual axis. Observing the quality of Placido disc mires is useful in understanding the wettability of the scleral lenses. Placido disc reflections will dictate where to decenter optics of a multifocal lens on a decentered scleral lens (Figures 2A, 2B).
Pachymetry
Figure 3. OCT epithelial thickness map showing forme fruste keratoconus. Morphology of epithelial cells is often the first to change in early-stage disease. Notable is the difference in midperipheral epithelial thickness superonasally (50-51 µm) as compared with inferotemporally (47-48 µm). (Image courtesy of Jeffrey Sonsino, OD, FAAO)

Just as topography is used to manage the underlying disease, so too is pachymetry. Pachymetry is especially useful in monitoring the stage of progressive diseases such as keratoconus. Epithelial thickness maps can be used to detect keratoconus earlier than other objective measures.6 Pachymetry is also very helpful in monitoring the thickness of a corneal graft with scleral lenses. A baseline should be taken before scleral lens fit. If thickness increases over time, the provider should increase the Dk value of the lens material, decrease lens thickness, or tightly control the vault to 200 µm (Figure 3).7
Optical coherence tomography
Optical coherence tomography (OCT) is by far the most important tool for evaluating scleral lenses. We strongly believe that sclerals cannot be properly managed without it. Once a trial lens is selected and inserted on the patient’s eye, anterior segment OCT (AS-OCT) is used to take high-resolution, cross-sectional images of the central clearance, limbal clearance, and landing zone of the scleral lens on the sclera.
First, a central line scan is taken to measure vault. The fact that we now know that increasing vault from 200 µm to 400 µm results in 30% less oxygen reaching the cornea tells us that precision is king with our fitting philosophy.8 It is no longer acceptable to fit with a loose range in vault. In most hands, the slit beam estimation technique simply cannot provide the precision required with modern fitting techniques. Likewise, fluorescein evaluation is useless when observing a lens on the eye after many hours of wear.
Next, line scans are taken at the limbus in each of the principal meridians of the lens. This line scan will show both limbal vault and haptic alignment. Since most of our scleral designs use toric haptics, the line scans are taken after observing the toricity marks at the slit lamp and lining up the AS-OCT with the hash marks, and then 90° away, for a total of 4 scans. If there is an irregular condition, such as corneal (limbal) nodules, pinguecula, blebs, or symblepharon, many more line scans may be indicated.
Wavefront aberrometry
Figure 4.Higher-order aberration (HOA) typically becomes problematic for patients when they exceed 1D. This is the display on a VX-130 wavefront aberrometer. In this example, the lower-order aberration (1.10D OD, 1.75D OS) is correctable with a spherocylindrical overrefraction. The HOA (0.15D OD, 0.16D OS) becomes irrelevant after the overrefraction is incorporated into the lens. (Image courtesy of Jeffrey Sonsino, OD, FAAO)

We use “overaberrometry” on all scleral lens fits by taking wavefront aberrometry measurements through the scleral lens. A wavefront aberrometer yields more information about the overrefraction than a traditional autorefractor. It can discriminate and classify aberrations into lower and higher order. Lower-order aberrations are easily corrected in a scleral lens using a spherocylindrical overrefraction. Higher-order aberration signals a lens fit problem, a poorly wetting surface, or internal astigmatism (Figure 4).
Scleral topography
A study conducted by first author Gregory DeNaeyer, OD, FAAO, and a team of investigators showed that approximately only 5% of sclera are spherical.9 With irregular sclerae in the majority of the population, it can be helpful to map that irregularity. Some lens manufacturers report better fitting with a more customized scleral alignment. However, the majority of patients should be able to be fit well with standard toric haptics.
Impression-based technology
When using the standard trial-and-error method to fit sclerals, the fitting process can take 4 to 6 visits, with an average of 2.8, to get the optimal lens for each eye.10 An impression-designed scleral lens uses an impression of the cornea and the sclera to create a computer-aided design (CAD) image of the ocular surface. A lens is then designed based on the CAD image to fit perfectly, even with the most irregular sclera. This technique creates the most custom-fit lenses, allowing for rotational stability by properly fitting over all lumps and bumps of irregular sclerae. This technology can also be useful when patients travel long distances for their care and yields the least number of follow-up visits.
Experience
Once you have acquired the training and equipment necessary to fit at a high level, perhaps the most difficult aspect of developing expertise is gaining the requisite experience in the field. This can only come from experience seeing the right types of patients. If you are in partnership with a cornea specialist who tends to see patients who require scleral lenses, your task is somewhat easier. If you have a general practice, then it will take time to develop a reputation for tackling difficult cases. However, you can start by mining your current patient population. The 2 ways that have proven successful are using your electronic medical record for diagnosis and contacting your GP lab for types of lenses. Find all the patients with keratoconus in your practice and refit them from corneal GPs into sclerals. They will thank you for this.
Be very careful before soliciting referrals from other providers in your area. Only after you have developed the experience to properly tackle all the cases that come your way should you reach out to colleagues. You don’t want even 1 of your patients reporting to their referring doctor that you were having difficulty with their fit.
With experience, you will learn how to incorporate scleral lens patients efficiently into your practice flow. Set aside more time for scleral lens appointments than you would a comprehensive eye examination. Teach your techs how to complete the ancillary testing and even the fitting process. It helps if they can complete overrefractions for you. Schedule return scleral lens patients every 2 weeks until the fit process is complete. We tell all our new scleral lens patients that it will take 4 to 6 visits to complete the process, but in subsequent years, the process is much quicker. When we set expectations like this, patients are rarely upset at our insistence on refining the fit.
Experience will teach you how to get the most out of your chosen scleral lens designs. Your laboratory consultants will work with you day after day so that you learn how to customize the design. All modern lens designs are great when you know how to tweak them. With investments in training, equipment, and experience, all of us can get there.
References
Woo University. What’s next? the future of scleral lenses. Woo University YouTube page. Published May 22, 2023. Accessed January 29, 2024. https://www.youtube.com/watch?v=n28CSiqUvpQ
Accreditation Council on Optometric Education Accredited Professional Optometric Degree Programs. American Optometric Association. Report. Published July 18, 2022. Accessed February 5, 2024. https://www.aoa.org/AOA/Documents/Education/ACOE/od_directory_%202020_12_01.pdf
Online curriculum: lecture series for educators. GP Lens Institute. Accessed February 6, 2024. https://gpli.info/online-curriculum/
Sonsino J. How patients benefit from “Navy Seal training for optometrists.” Optique. Accessed February 13, 2024. https://www.optiquenashville.com/how-patients-benefit-from-navy-seal-training-for-optometrists/
Scleral Consultative Instituteto present elite scleral lens fitting and practice management training for select optometrists. ABB Optical Group. Accessed February 5, 2024. https://www.abboptical.com/sites/default/files/pdf/Bootcamp-Flyer.pdf
Yang Y, Pavlatos E, Chamberlain W, Huang D, Li Y. Keratoconus detection using OCT corneal and epithelial thickness map parameters and patterns. J Cataract Refract Surg. 2021;47(6):759-766. doi:10.1097/j.jcrs.0000000000000498
Michaud L, van der Worp E, Brazeau D, Warde R, Giasson CJ. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012;35(6):266-271. doi:10.1016/j.clae.2012.07.004
Giasson CJ, Morency J, Melillo M, Michaud L. Oxygen tension beneath scleral lenses of different clearances. Optom Vis Sci. 2017;94(4):466-475. doi:10.1097/OPX.0000000000001038
DeNaeyer G, Sanders D, van der Worp E, Jedlicka J, Michaud L, Morrison S. Qualitative assessment of scleral shape patterns using a new wide field ocular surface elevation topographer. J Cont Lens Res Sci. 2017;1(1):12-22. doi:10.22374/jclrs.v1i1.11
Schornack MM, Patel SV. Scleral lenses in the management of keratoconus. Eye Contact Lens. 2010;36(1):39-44. doi:10.1097/ICL.0b013e3181c786a6