- Digital edition: January 2022
- Volume 14
- Issue 01
A narrative guide for cataract postoperative surgical care
Expected findings in follow-up, management, and potential complications.
Patient case
An 84-year-old man arrives to your clinic for his 1-day postoperative visit after undergoing uneventful right eye cataract surgery.
You begin your exam with a thorough history that may suggest a complication.
He reports that his vision is mildly blurry, but better than before surgery. He is mildly photophobic and he has a mild foreign body sensation OD.
He says he has been adherent with his combination drop (prednisolone phosphate/gatifloxacin/bromfenac), and that he slept well the night prior with his Fox shield.
It was anticipated for him to use his drop 4 times a day for 1 week, then twice a day for 1 week, once a day for 1 week, and then discontinue use.
While cataract extraction is generally considered a low-risk procedure, there are potential adverse outcomes—such as infectious endophthalmitis, retained lens fragments, vitreous wick, iris prolapse, toxic anterior segment syndrome, macular edema, or retinal detachment—that may make recovery more challenging.
Additionally, certain medications can complicate cataract surgery.
Related:
The most concerning medications include current or previous use of alpha receptor blockers such as tamsulosin (Flomax), terazosin hydrochloride (Hytrin), doxazosin (Cardura), and alfuzosin (Uroxatral) because they make intraoperative floppy iris syndrome more likely to occur.
Thankfully, the patient had no history of taking an alpha receptor blocker.
His only systemic diagnoses were hypertension, which was well controlled with hydrochlorothiazide (Microzide), and hypercholesterolemia, which was controlled with simvastatin (Zocor).
The frequency with which you see your patient during the 90-day cataract postoperative period varies case by case, but for uneventful surgical cases where the patient heals appropriately, it is safe to have them come in for follow-up at 1 day, 1 week, and 1 month postoperatively.
Expected 1-day findings
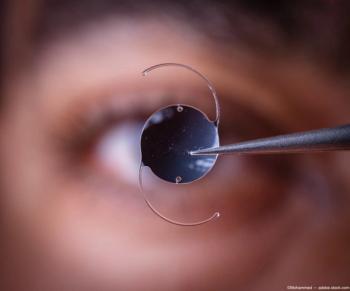
Expected findings during the 1-day postoperative visit include a visual acuity between 20/20 and 20/60, residual dilation, a mildly elevated intraocular pressure (IOP), a small ptosis from the spring clamps used during surgery, conjunctival injection, conjunctival hemorrhage, mild punctate keratitis, mild corneal edema surrounding the incision site, “snail tracks” of the corneal endothelium, and mild anterior chamber cells, flare, and capsular debris.
Common symptoms include a foreign body sensation, mild pain, dryness, grittiness, mild discomfort, photophobia, mild headache, poor sleep the night prior, and blurry vision.
There are numerous postsurgical complications to keep in mind during the 1-day postoperative visit, including corneal abrasions, wound leakage, elevated IOP (iatrogenic), iris prolapse, vitreous wick, toxic anterior segment syndrome (TASS), infectious endophthalmitis, retained lens fragments, decentration of the intraocular lens (IOL), and posterior capsular opacification.
Related:
In this case, the patient has an uncorrected visual acuity of 20/60, which is pinholed to 20/302 OD. His extraocular muscles are full without pain and confrontation visual fields are full to finger counting in all quadrants OD. His pupils are equal, round, and reactive to light without an APD.
Upon anterior biomicroscopy, he has trace diffuse bulbar conjunctival injection, 1+ microcytic edema of the cornea at the temporal incision site, 1+ diffuse corneal edema, and mild corneal endothelial folds superiorly to the visual axis.
His anterior chamber has 2+ cell, 0.5+ flare, and mild debris. His posterior chamber-IOL (PC-IOL) is centered and clear. His IOP is measured to be 35 mmHg OD, and the wound does not reveal negative staining, which might indicate a positive Seidel sign. All other findings are within expectations for 1 day after surgery.
Iatrogenically elevated IOP is common (22%) during the 1-day postoperative visit, and there are 2 options to be considered for lowering the pressure: an ocular hypotensive drug or burping the wound.1
The patient did not endorse a headache, nausea, or vomiting, so 1 drop of 0.5% timolol maleate, a fast-acting ocular hypotensive, is instilled in-office OD. Twenty minutes later, his IOP measured 22 mm Hg.
Related:
He is prescribed 0.25% timolol maleate QAM OD, and is instructed to continue his combination drop regimen as specified above and continue wearing his Fox shield OD nightly for the next week to prevent inadvertently reopening the wound while sleeping.
Additional instructions are provided to aid in not reopening the wound, including avoiding heavy lifting, bending at the hip, and rubbing his right eye. To impede infection, he is educated to avoid getting water in his right eye while showering.
He is educated on symptoms such as pain, discharge, decreased vision, increased photophobia, increased redness, new floaters, new photopsia, or a curtain over his vision, which may indicate an infection, retinal detachment, or IOP spike.
Expected 1-week findings
During the 1-week postoperative visit, clinical findings should be stable or improved compared with the 1-day visit. There may be a mild residual anterior chamber reaction and mild corneal edema at the incision site. Patients typically report an improvement in vision, but they may have mild photophobia and glare.
Assessing the integrity of the incision site is crucial at this visit to guide future management plans, such as bathing instructions and restrictions on physical activity.
The patient is seen for his 1-week postoperative visit, upon which he reports his eye feels normal, and that he has adhered to his drop regimen and wearing his Fox shield. His uncorrected VA is improved to 20/25-. All other preliminary testing is normal.
Related:
On anterior segment biomicroscopy, his wound is healing nicely and there is no staining over the wound, just residual trace edema at the incision site.
His anterior chamber is now deep and quiet. His IOP is lowered to 12 mmHg, so the timolol is discontinued. Since there is no staining over his incision, he is now able to shower normally and discontinue using the Fox shield. All other education stays the same.
Expected 1-month and 3-month findings
When the patient returns for his 1-month and potentially his 3-month visit, the eye should be completely normal except for an incision scar.
Some late-stage complications can include posterior capsular opacification, cystoid macular edema, a retinal break, or a retinal detachment.
At the patient’s 1-month postoperative visit, he reports that his right eye feels normal and that he is able to see well at distance. His uncorrected VA is improved to 20/20- and he refracts to +0.25 -0.25 x 180 with a +2.50 add.
On anterior segment biomicroscopy, all findings are normal with the addition of a corneal incision scar temporally. His IOP remains normal at 11 mm Hg and upon dilation all posterior segmenting findings are normal OD. No other positive tests are detected.
He is then discharged from care; however, he is educated to return to clinic if any ocular disturbances were noted.
----
References
1. Kim JY, Jo MW, Brauner SC, et al. Increased intraocular pressure on the first postoperative day following resident-performed cataract surgery. Eye (Lond). 2011;25(7):929-936. doi:10.1038/eye.2011.93
2. Hayashi K, Tsuru T, Yoshida M, Hirata A. Intraocular pressure and wound status in eyes immediately after scleral tunnel incision and clear corneal incision cataract surgery. Am J Ophthalmol. 2014;158(2):232-241. doi:10.1016/j.ajo.2014.04.018
3. Durand, ML. Bacterial and fungal endophthalmitis. Clin Microbiol Rev. 2017;30(3): 597-613. doi:10.1128/CMR.00113-16
Articles in this issue
about 4 years ago
Mitigate diabetic retinopathy with early improved glucose controlabout 4 years ago
Quiz: Postoperative careabout 4 years ago
Incorporating injections into your practiceabout 4 years ago
The safety and efficacy of mass-produced colored contact lensesabout 4 years ago
Case study: persistent keratitis OS presents in 68-year-old womanNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.