All about red caps: Mydriatics and cycloplegics

Roya Attar, OD, MBA, FAAO

Do you ever wonder what the difference is among all those bottles with the red caps you use in your office for dilating patients? Each has a different name and different concentration-but as far as you can tell, they all serve the end purpose of dilating patients.
Dilation explained
Dilation is an important aspect of a comprehensive eye exam and serves both diagnostic and therapeutic purposes.
Dilation aids in improved visualization of the fundus and an increased detection rate of abnormalities. Pharmacological dilation is generally required for a thorough evaluation of ocular structures. Dilation is usually achieved through a pharmaceutical agent.1,2
In most eyecare offices today, there are several options when it comes to dilating patients, each with a red cap. It is crucial to understand the differences among each dilating agent as well as the risks and benefits of each.
Techs likely have heard the words “mydriatic” or “cycloplegic” used when referring to dilation. A mydriatic is an agent that induces dilation of the pupil or mydriasis, whereas cycloplegia refers to paralysis of the ciliary muscle, thereby inhibiting accommodation or focusing ability.2-4Related: The case of the single fixed pupil
How dilation works
Before getting into the nitty-gritty of the pharmacology of dilation drops, let’s briefly review ocular anatomy and the structures involved in the dilation process.
Pupillary dilation is controlled through the autonomic system which consists of the sympathetic and parasympathetic pathway.
Two opposing muscles in the iris-the sphincter and the dilator-are under the control of the autonomic nervous system. The sympathetic pathway leads to the dilator muscle of the iris, while the parasympathetic pathway leads to the sphincter muscle of the iris.
This is important because each drop’s mechanisms of action affects one of the pathways.
Tropicamide, cyclopentolate, atropine, homatropine, and scopolamine work by inhibiting the pupillary sphincter which causes mydriasis and inhibits the ciliary body-thisleads to cycloplegia through the parasympathetic pathway. These drops are known as cholinergic antagonists or anticholinergics which denotes their mechanism of action to stop the effects of acetylcholine by binding to and inhibiting cholinergic receptors.2-4
Related: Digital fundus cameras feature mydriatic, nonmydriatic functions
Drop by drop
Tropicamide is considered clinically the drug of choice for routine dilation because it has the fastest onset and shortest duration of action-it quickly gets your patients dilated and its dilation effects quickly wear off.
It is offered in two concentrations, 0.5% and 1.0%. Both have the same mydriatic effect, but the 1.0% concentration has a greater cycloplegic effect. Side effects include stinging upon instillation and transient increase intraocular pressure (IOP) in primary open-angle glaucoma (POAG) patients. There are no direct contraindications to tropicaminde except in cases in which a patient may be allergic to the drops.2,4-7
Cyclopentolate is the drug of choice clinically for routine cycloplegic refraction because it provides for a faster cycloplegia with less residual accommodation. It is often used for pediatric patients and certain patients with accommodative disorders, such as accommodative excess or accommodative spasm.2-4,6
Atropine is the most potent mydriatic/cycloplegic available. It is directed for use when complete cycloplegia is required. Because of its potency and long duration of action, it is not routinely used for dilation. Atropine is indicated in cases of suspected accommodative esotropia and for amblyopia treatment.3,4
Related: Patching, atropine may suit moderate or severe amblyopia
Although rare, atropine toxicity is a potential side effect. Symptoms of atropine toxicity include dry mouth, usually the first sign; dry flushed skin; rapid pulse; disorientation; and fever due to central nervous system effects on the hypothalamus. Special consideration and precautions must be taken when treating small children, elderly, and Down syndrome patients.3,4
Homatropine is not routinely used for dilation. It has a weak but prolonged cycloplegic effect and a strong mydriatic effect, making it suitable for uveitis therapy. It serves as the standard for treating anterior uveitis because it is useful in minimizing pain and for prevention of posterior synechiae. These benefits are obtained with minimal cycloplegic effects, unlike atropine.4,8
Scopolamine is also not routinely used or found in most doctor’s offices. It is reserved for use in patients who may be allergic to other agents. Central nervous system side effects are more common because it more easily crosses the blood-brain barrier. Special consideration and precautions must be taken when treating small children, elderly, and Down patients.4
Related: Know how to care for pediatric patients diagnosed with Down syndrome
Another category of dilating drops affects the sympathetic system by stimulating the iris dilator muscle leading to mydriasis.
Phenylephrine is the most commonly used drug in this category. It is available in a 2.5% and 10% solution. The 10% strength produces an increase in rate but not magnitude of mydriasis and is useful for breaking posterior synechia. Phenylephrine alone will provide for dilation without cycloplegia. It is often used in combination with anticholinergics to produce maximal dilation of the pupil.9
There is a risk of adverse cardiovascular events with phenylephrine, which have been more frequently reported with the 10% strength, therefore the 2.5% solution is recommended for routine use and in infants and the elderly. Phenylephrine should be avoided in atropinized patients. The 10% strength should be used with caution in patients with cardiac disease, orthostatic hypotension, hypertension, aneurysms, type 1 diabetes, and advanced arteriosclerosis. Phenylephrine is contraindicated in patients taking MAO inhibitors, tricyclic antidepressants, reserpine, guanethidine, or methyldopa. Possible ocular side effects include mild stinging and pigmented aqueous floaters. Possible systemic side effects include acute systemic hypertension, ventricular arrhythmia, tachycardia, and subarachnoid hemorrhage.3,4
Paremyd (Akorn) is another commonly used dilating drop. Paremyd is a combination drop, 1% hydroxyamphetamine solution combined with 0.25% tropicamide. Thus the drug works on both the parasympathetic (sphincter) and sympathetic (dilator) systems of the eye.3,4,7
Related: The proper procedure for testing pupils
Administering dilating drops
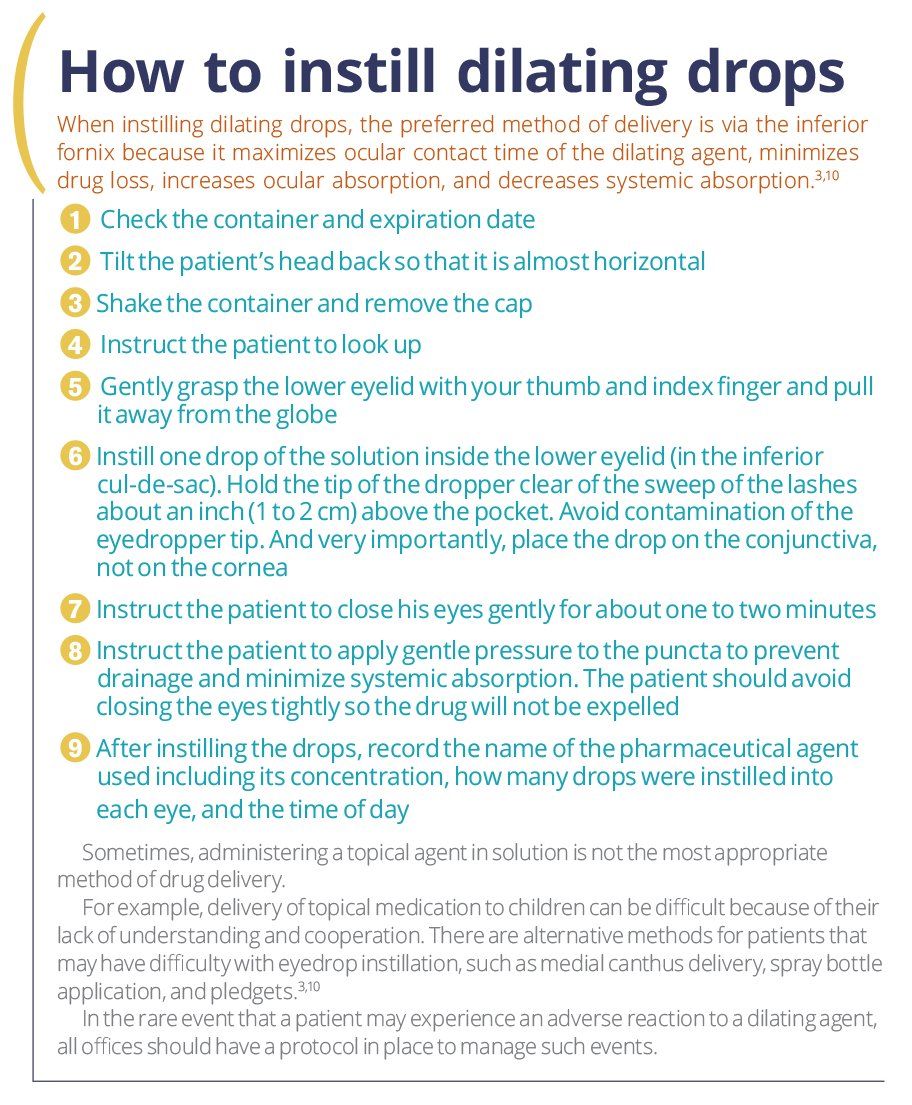
Equally as important as knowing the differences among the dilating drops in the office is how to administer them.
The goal of proper eye drop instillation is to deliver a full dose of the drug to the eye while minimizing systemic exposure and maximizing patient safety and comfort.
Prior to instilling dilating drops, it is important to educate the patient about what is happening and why. Advise patients of the purpose of dilation as well as possible side effects, which include:3,10
• Blurred vision, especially for near tasks
• Photophobia (light sensitivity)
• Decreased ability to recognize low-contrast hazards
• Increased glare sensitivity
• Possible impaired aspects of driving and vision performance
• Potential angle closure in patients with narrow anterior chamber angles
Many offices ask patients to sign informed consent documents; however, even with signing such forms the patient record should include a note that the patient was educated. Equally as important to note in a patient’s chart is if the patient refused dilation. I suggest including additional documentation noting that the importance of dilation was stressed to the patient and schedule the patient to return on a separate visit for a dilation when necessary.
Related: How I built a customer service-centered practice
Prior to instilling dilating drops, make sure to wash/sanitize your hands-this goes for any time you perform a procedure that requires direct contact with a patient where you are not wearing gloves.10 It is also good practice to ensure that the patient observes you washing and/or sanitizing your hands.
Some practices advocate use of ocular anesthetics prior to dilation. Although not necessarily required, ocular anesthetics such as proparacaine help to decrease patient discomfort by reducing burning or stinging produced by instillation of the dilating agent. The anesthetic also decreases blinking and tearing and changes the permeability of the epithelium to the dilating agent, thereby maximizing drug penetration through the cornea.11,12
Wrapping up
Dilation is an integral part of a comprehensive eye exam. All practitioners and technicians should be aware of all of the dilating agents available today, their uses, as well as the possible risks and benefits of each.
Read more iTech content here
About the author
Roya Attar, OD, MBA, FAAO received her Doctorate of Optometry degree at the Rosenberg School of Optometry in 2013. She previously served as faculty and director of professional relations while at the Kentucky College of Optometry. Most recently, she became the first optometrist to be hired at the University of Mississippi Medical Center where she provides clinical services in addition to training and lectures for ophthalmology residents.
RoyaAttar@outlook.com
References:
1. AOA Evidence-based optometry guideline development group. Evidence-Based Clinical Practice Guideline. Comprehensive Adult Eye and Vision Examination. American Optometric Association. St. Louis, MO; 2015. Available at www.aoa.org.
2. Ihekaire DE. The comparative efficacy of cyclopegic drugs-tropicamide and cyclopentolate on school children. Int J Sci Res Edu. 2012;5(3):223-246.
3. Benjamin WJ. Borish’s Clinical Refraction. 2nd edition. St. Louis, MO: Butterworth-Heinemann; 2006. Print.
4. Bartlett JD, Janus SD. Clinical Ocular Pharmacology. 5th edition. St. Louis, MO: Butterworth-Heinemann; 2008. Print.
5. Lam PTH, Chan CKM, Rao SK, Fan DSP, Lam DSC. Randomized clinical trial on the efficacy and side effects of tropicamide and phenylephrine in mydriasis for ophthalmoscopy. J Optom. 2010;3(1):37-43.
6. Yazdani N, Sadeghi R, Momeni-Moghaddam H, Zarifmahmoudi L, Ehsaei A. Comparison of cyclopentolate versus tropicamide cycloplegia: A systematic review and meta-analysis. J Optom. 2018;11(3):135-143.
7. Cooper J, Feldman JM, Jaanus SD, Appleman W, Appel S, Horn D. Pupillary dilation and funduscopy with 1.0% hydroxyamphetamine plus 0.25% tropicamide (Paremyd) versus tropicamide (0.5 or 1.0%) as a function of iris and skin pigmentation, and age. J Am Optom Assoc. 1996 Nov;67(11):669-75.
8. Belliveau MJ, Arthur BW. Dilating pupils. CMAJ. 2011 Sep 6;183(12):1400.
9. Anderson HA, Bertrand KC, Manny RE, Hu Y-S, Fern KD. Comparison of two drug combinations for dilating dark irides. Optom Vis Sci. 2010 Feb;87(2):120-4
10. Carlson NB, Kurtz D. Clinical Procedures for Ocular Examination. 4th edition. New York: McGraw-Hill Education; 2004. Print.
11. Haddad DE, Rosenfield M, Portello JK, Krumholz DM. Does prior instillation of a topical anaesthetic alter the pupillary mydriasis produced by tropicamide (0.5%)? Ophthalmic Physiol Opt. 2007 May;27(3):311-4.
12. Siderov J, Chuang SM, Ian K, Prassinos G, Tziortzi E, Wong JY. Effect of proparacaine on tropicamide-induced mydriasis. Optom Vis Sci. 1997 Dec;74(12):1039-43.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.