Become the best tech for your patient
Follow CARE to value patients as individuals and build trust
As a fellow technician, I always carry myself in a manner of respect, courteousness, empathy, and attentiveness. I allow patients to feel valued as an
individual-not just a chart number.
Keeping these traits top of mind during your clinic day will lead to a great experience for your patient, which will build an amazing rapport that will lead to trust from the patient.
Related:
I developed important key factors of what a technician should know for their interactions. I use the acronym CARE:
– Care
– Attention
– Responsiveness
– EmpathyConfidence
Take pride in your appearance; having a clean uniform or professional attire shows that you are serious about yourself and your work.
Learn all medical conditions, and become familiar with all medications and their side effects. This will help you determine what testing is required. This comes across to the patient that you know what you are doing, and in that moment, trust is developed, giving the patient the reassurance that she came to the right place.
Technicians should obtain their knowledge of the field through studying or taking CE (continuing education) courses. The more information we know, the better we can help service our patients properly. That way, the physician has all the necessary tools they need to better diagnose and treat the patient.
Attention
Pay attention to your patient’s movement or mannerisms. Especially for established patients, changes may indicate something new going on
systemically or a recent injury.
Give your patient your undivided attention and make her feel valued. I know complete attention is more difficult with the advent of electronic medical records (EMR), but it goes a long way when you acknowledge your patient as a person instead of a chart number.
It is important that technicians don’t lose sight of the human interaction; that is the essence of health care.
Listening to the patient’s chief complaint and history of present illness (HPI) and taking a thorough history- including all medications-is key. This will inform how to move forward with testing.
This information will also drive the examination and what steps will be required to follow-up with what was discussed.
It will also allow you to start thinking like a clinician and not just a technician going through the motions.
Empathy
Doctor’s offices tend to make patients uncomfortable. Sometimes patients get the feeling of coldness and indifference from the office and its staff, which makes patients not want to be there.
Make the patient's experience enjoyable. Greet every patient with a smile, convey that you are happy to have them come to the office. Show empathy and establish a rapport with patients, especially elderly patients who may need help moving around. Offer help, especially if they come to the visit without a companion.
Some patients might be going through difficult times that you know nothing about, so try to be understanding and, in a sense, read the situation.
Being a healthcare professional means you have a career in helping people and making a difference. It shouldn’t be viewed as simply a paycheck or a way to pay the bills. I got into the field to help people and make a difference in someone’s life other than my own. I like to view every single person in my exam chair as a family member, friend, and-more importantly-myself.
Related: 3 patient scenarios show triage doesn't need to be traumatic Case example
I had an experience many years ago with a new patient, a 55-year-old male whose chief complaint was blurred vision and eye fatigue. I proceeded with gathering a past ocular history (POH), past medical history (PMH), surgical and family histories, and a review of systems (ROS).
The patient had no corrective eyewear for distance or near acuity. When checking visual acuity, I noticed he was consistently missing the first and last letters of the Snellen chart. With pinhole, he corrected to one line more but still couldn’t fully see the whole line. I then refracted the patient and encountered the same occurrence.
Upon further examination, confrontational visual field (CVF) yielded bilateral restriction in temporal field, extraocular muscles (EOM) were full, and Amsler grid was blurred without distortion. Pupils were round and normal, and no afferent pupillary defect (APD) was found.
On slit lamp exam, corneas were clear, anterior chamber was deep and quiet, and trace nuclear sclerosis was found. Intraocular pressures (IOP) were over 20 mm Hg in both eyes.
Related:
I considered possible glaucoma, but the patient had no family history. I treated this case as a glaucoma work-up.
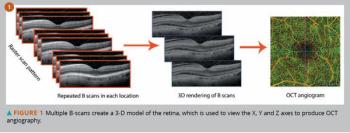
Pachymetry showed the reading of the microns as thick and helped to lower IOP to high teens. Automated perimetry, dilation, and optical coherence tomography (OCT) of the optic nerve were performed.
I came across a troubling view on the visual field results. I presented it immediately to the physician, and he determined it was bitemporal hemianopsia. Viewing the OCT, the retinal nerve fiber layer (RNFL) was within normal limits, and macula was clear of fluid.
The physician sent the patient for a brain magnetic resonance image (MRI). Results showed a substantial tumor in the patient’s optic chiasm. The patient was referred to a neurosurgeon who immediately performed surgery. The neurosurgeon said if the tumor had not been found, it may have caused the patient's death.
Months later, the patient followed up with our office and was extremely grateful. He believed he was able to have an extended life and preserved vision because of the care he received from us.
Related: Teaching skills for successful technicians Moving head
You will come across countless scenarios with your patients-whether due to their present illnesses, current medications, and new concerns. We as technicians are the front lines, the ones who start the exam for the physician.
It is our job to identify concerns prior to the exam and relay them to the physician. If you have the comfort level from your physicians to perform testing with what you saw in your exam and relay your findings to the physician, they view you as a clinician, not a technician.
It is about the passion to keep educating yourself and to never stop learning. It is also the passion to want to better yourself by becoming certified in the field and advancing skill levels in the examination. Think outside the box, and start thinking like your doctor would think.
Keep in mind we are all in this field to help make a difference in someone’s life by showing her that we care about her and her well-being as well as her visual and ocular health.
If you follow these key points, you are on your way to becoming the best technician for your patient.
Read more iTech content here
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.