Case report: Don’t be misled by diabetic retinopathy

Despite the advancement in diagnostic technology and treatment strategies, diabetic retinopathy remains a major cause of new onset blindness in the U.S. According to Centers for Disease Control and Prevention (CDC), more than 650,000 of the 4.2 million Americans with diabetic retinopathy (DR) have vision-threatening DR (VTDR).1
VTDR, also referred to as sight-threatening diabetic retinopathy, is defined by the presence of diabetic macular edema or retinal neovascularization that are vision threatening. Either, if not closely monitored and/or treated, can lead to irreversible vision loss. Additionally the Vision Health Initiative (VHI) Report by the CDC indicates that the rate of Americans aged 40 years and older with DR and VTDR will triple from 2005 to 2050.1
Related: When to refer patients with diabetic retinopathy
With a high and rising incidence of DR and VTDR, eyecare providers in any practice mode will encounter patients who knowingly or unknowingly have diabetes and may suffer from DR of any level.
Stages of diabetic retinopathy have been classified by several classification schemes, with the two most common being International Clinical Diabetic Retinopathy Disease Severity Scale2 and Early Treatment of Diabetic Retinopathy Study (ETDRS).3
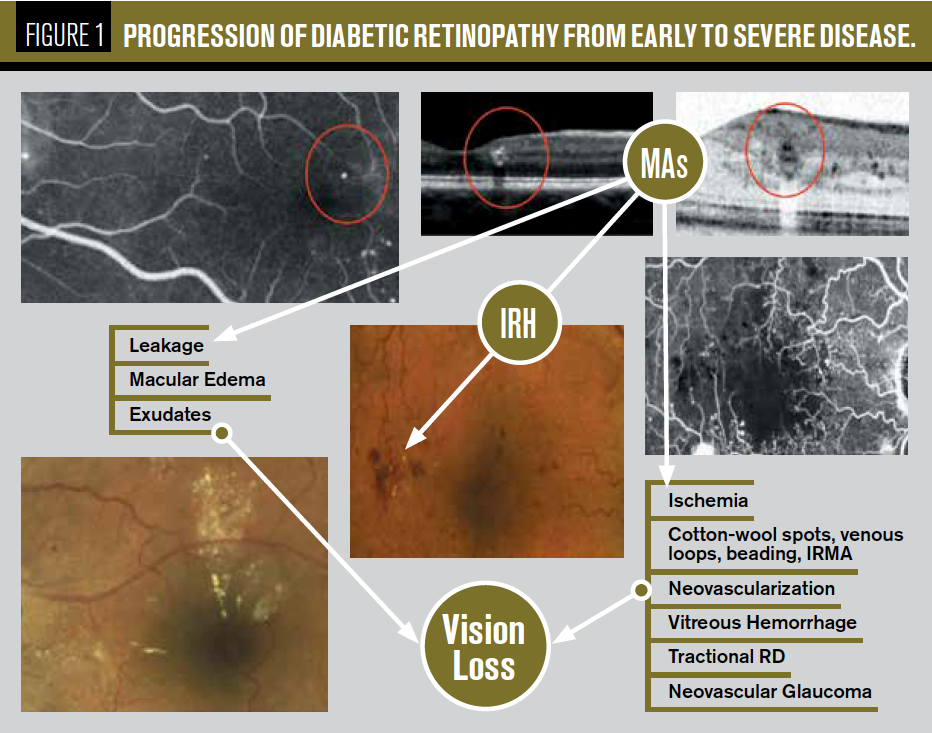
Regardless of the classification scheme, diabetic retinopathy is first clinically defined by the presence of microaneurysms (MAs), which are small outpouchings of retinal capillaries. Table 1 illustrates the progression from early DR to more advanced/VTDR.
Also by Dr. Mohammad Rafieetary: What we can learn from managing diabetic patients
Therefore, when a patient first presents with VTDR (see Figure 1), we must consider that this process began with an early, less aggressive/more treatable form, perhaps with few MAs (see Figure 2).
Conversely, when we detect a few MAs (Figure 2) we should consider that if not properly managed, the disease may progress to more severe stages with visual consequences (Figure 1).
Related: Using imaging to manage diabetic retinopathy
Case report
A 47-year-old white female is seen for examination with no chief complaints. She has a past medical history of type 1 diabetes mellitus, diagnosed 34 years ago, with recent hemoglobin A1C of 6.9; essential hypertension, diagnosed 20 years ago, well-controlled on medication; and obesity.
Medications include furosemide 20 mg tablet, lisinopril 2.5 mg tablet, metoprolol tartrate 25 mg tablet, naproxen 500 mg tablet, insulin aspart 100 unit/mL solution, potassium chloride 10 mEq tablet extended release, and vitamin D2 50,000 unit capsule.
On physical exam, visual acuity was 20/20 in each eye, intraocular pressures were OD 19 mm Hg and OS 20 mm Hg. All other anterior segment findings were normal with the exception of trace nuclear sclerosis bilaterally.
Undilated fundus exam was remarkable for a few MAs with no macular edema, which was confirmed with optical coherence tomograghy (OCT) (Figure 2).
Bases on this retinal examination finding, this patient can be diagnosed with mild nonproliferative diabetic retinopathy (mild NPDR) without macular edema (International Clinical Disease Severity Scale for DR2).
Related:
If this was a patient under your care, what would you do next?
• Patient education and follow-up in one year
• Patient education and follow-up in 6 months
• Dilate the patient at this visit or on follow-up exam made shortly after this first examination
• Refer patient to retina specialist
Dilated fundus exam is remarkable for more MAs and intraretinal hemorrhages (IRH) mainly in the mid- and peripheral retina (see Figure 3).
Based on this information, this patient can be diagnosed with moderate NPDR.
How would you manage this patient now?
See what happens with further investigation. Fluorescein angiography is obtained, which reveals a more concerning picture with presence of capillary nonperfusion and neovascularization everywhere (NVE).
Based on this constellation of findings, the patient should be classified as proliferative diabetic retinopathy (PDR), which is a vision-threatening stage.
Related: Proliferative retinopathy leads to risk of vision loss
Discussion
Diabetic retinopathy, regardless of staging, can be challenging to correctly categorize and manage. Clinicians and patients alike face several barriers to proper screening and management of diabetic retinopathy.
These barriers are even more pronounced when patients are still at a stage of their disease course in which they are visually asymptomatic.
A systematic review identified lack of knowledge, attitude, awareness, and motivation as major barriers to appropriate eye care in this context. Enablers, meaning factors that enable one to seek out appropriate medical care, included fear of blindness, proximity to screening facility, experience of vision loss, or concern for ocular complication.4
More than 70 percent of the studies included in the Piyasena et al review included patients of high income setting.4 One could speculate that the negative impact of these barriers are more profound and the positive impact of enhancers is diminished in the lower socioeconomic class.
Aside from concerns pertaining to access to care, correction classification of disease remains a diagnostic challenge for clinicians.
Related: Pros and cons of using an AI-based diagnosis for diabetic retinopathy
In the example of our case patient, incorrect classification (diagnosing this patient with moderate NPDR as opposed to PDR) will lead to lack of timely treatment (observation as opposed to panretinal photocoagulation/anti-VEGF) as well as an inappropriate follow-up interval (three to six months as opposed to one month).
During this follow-up interval, this patient may develop further complications such as vitreous hemorrhage or tractional retinal detachment that could have been minimized with more timely treatment.
While classification systems of nonproliferative and proliferative DR have been well validated based on presence of certain retinal lesions, the rate of progression to vision-threatening diabetic retinopathy is less predictable.5 Guidelines have been published for appropriate timing of follow-up and whether referral to a retina specialist is indicated based on disease severity.6
However, strict adherence to guidelines without consideration of risk to progression of VTDR (such as patient history of noncompliance, missed appointments, status of the fellow eye) may lead to infrequent follow-up for patients at high risk for progression and too frequent follow-up for those with low risk of progression to VTDR.5
Thus, management of these patients should be tailored to the patient, not solely guideline-driven.
Read more about patient care
The complexity of DR assessment and management includes inadequate assessment, appeasing patients, and patients’ poor compliance to their medical regimen and follow-up eyecare. It is aided by existence of mitigating factors and comorbidities such as:
• Smoking
• Lack of exercise
• Poor dietary habits
• Obesity
• Systemic hypertension
• Lipid disorders
• Sleep apnea
• Cardiovascular disease
• Carotid artery disease
• Hematologic disorders such as anemia, renal failure
All of these factors need to be considered and/or investigated in proper management of patients with diabetes with or without DR. If properly addresses, DR does not have to be a “blinding” disorder because effective treatments battle this potential catastrophic condition.
In the case of this patient, fluorescein was considered due to longevity of diabetes compiled with HTN and obesity as well as the clinical finding of peripheral retinal hemorrhages.7
About the authorsDr. Mohammad Rafieetary is a Diplomate of the American Board of Optometry as well as the American Board of Certification in Medical Optometry. He has received numerous awards including Tennessee Optometrist of the Year and the National American Diabetes Association Award of the Achievement of Distinction. Dr. Rafieetary publishes and lectures on posterior segment disease. He has relationships with Notal Vision, Optos, Heidelberg, and Angigenisis Foundation
mrafieetary@charles-retina.com.
Dr. Salar Rafieetary graduated with honors with a B.S. in neuroscience from Rhodes College. He received his medical degree from the University of Tennessee Health Science Center, where he graduated with honors and served as the president of his class. He completed his transitional internship at Methodist University Hospital. After residency, he plans on pursuing fellowship training, likely in vitreoretinal surgery.
srafieet@uthsc.edu
References:
1. Centers for Disease Control and Prevention. Vision Health Initiative (VHI) Report. Available at: www.cdc.gov/visionhealth/publications/diabetic_retinopathy.htm. Accessed 5/10/19.
2. Wu L, Fernandez-Loaiza P, Sauma J, Hernandez-Bogantes E, Masis M. Classification of diabetic retinopathy and diabetic macular edema. World J Diabetes. 2013 Dec 15;4(6):290-4
3. Early Treatment Diabetic Retinopathy Study design and baseline patient characteristics. ETDRS report number 7. Ophthalmology. 1991 May;98(5 Suppl):741-756.
4. Piyasena MMPN, Murthy GVS, Yip JLY, Gilbert C, Zuurmond M, Peto T, Gordon I, Hewage S, Kamalakannan S. Systematic review on barriers and enablers for access to diabetic retinopathy screening services in different income settings. PLoS One. 2019 Apr 23;14(4):e0198979.
5. Sivaprasad S, Pearce E. The unmet need for better risk stratification of non-proliferative diabetic retinopathy. Diabet Med. 2019 Apr;36(4):424-433.
6. Wong TY, Sun J, Kawasaki R, Ruamviboonsuk P, Gupta N, Lansingh VC, Maia M, Mathenge W, Moreker S, Muqit MMK, Resnikoff S, Verdaguer J, Zhao P, Ferris F, Aiello LP, Taylor HR. Guidelines on Diabetic Eye Care: The International Council of Ophthalmology Recommendations for Screening, Follow-up, Referral, and Treatment Based on Resource Settings. Ophthalmology. 2018 Oct;125(10):1608-1622.
7. Nentwich MM, Ulbig MW. Diabetic retinopathy - ocular complications of diabetes mellitus. World J Diabetes. 2015 Apr;6(3):489-499.

Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.