- August digital edition 2020
- Volume 12
- Issue 8
How the tear film affects IOL measurements
Studies highlight importance of tear film stability in cataract and refractive surgery outcomes
An unstable tear film in cataract patients can affect the accuracy of IOL calculations and result in suboptimal refractive outcomes. It is therefore highly beneficial to pre-treat the ocular surface before obtaining any measurements in order to provide the best possible refractive outcomes.
Ocular surface health is important for all patients, but it is especially important in cataract and refractive surgery candidates—not only to minimize postoperative dry eye symptoms but also to optimize visual outcomes.
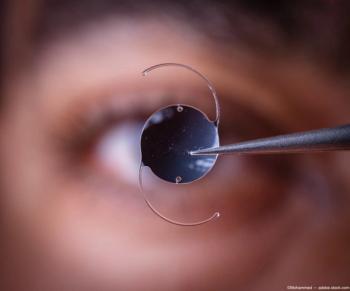
Nailing the refractive goal for those who pay for advanced technology implants is key for patient satisfaction. Intraocular lens (IOL) calculations are highly dependent on preoperative measurements. Consider: the tear film provides most of the refractive power of the eye. As such, it should come as no surprise that, in cataract surgery patients, an unstable tear film reduces the quality of corneal reflections and, therefore, can compromise K readings,1,2 which, in turn, can affect the accuracy of IOL calculations and result in suboptimal refractive outcomes.1-5
Failure to address problems with the tear film and ocular surface before surgery can negatively affect surgical outcomes and patient satisfaction. Therefore, it is extremely beneficial to pre-treat the ocular surface before obtaining measurements for surgery. Here, I will share results of two of my own pilot studies. The first demonstrates the effect of a single, 5-minute in-office, moist heat eye compress treatment on tear film stability, and the second demonstrates the effect of thermal pulsation on IOL measurements.
Moist heat compress study
In the first study, we sought to determine whether brief exposure tomoist heat eye compress therapy (Bruder) would have a significant effect on tear film stability, regardless of health, pre-existing conditions, or contact lens wear. A total of 27 patients (54 eyes) were evaluated in this analysis.
In addition to baseline diagnostics, Surface Qualifier image analyses (Cassini Technologies) were performed on all patients before and after the 5-minute treatment with moist heat therapy. The Surface Qualifier image displays the tear film with blocks and lines in seven quadrants. Regular yellow blocks and lines in all seven quadrants suggests a stable tear film, whereas irregular blocks and wavy or missing lines indicate an unstable tear film.
Three patients had a history of diabetes (6 eyes) and 7 (14 eyes) were contact lens wearers. Ten eyes (18.5 percent) tested positive on InflammaDry (Quidel) MMP-9, and 37 eyes (68.5 percent) had abnormal tear osmolarity at initial presentation. In total, 72 percent (39 eyes) of the total test sample presented with unstable tear film and 28 percent (15 eyes) had a stable tear film prior to the moist heat compress treatment.
Prior to treatment, 39 eyes had an unstable tear film, but nearly half of these eyes (49 percent) converted to stable tear film following a 5-minute treatment with the moist heat compress. In other words, patients with an unstable tear film were two times less likely to have an unstable tear film following short-term exposure to the compress. The healthy eye group consisted of 15 eyes with a stable tear film prior to treatment with the compress. This number jumped to 30 eyes following treatment.
Based on all eyes studied, patients were three times more likely to have a stable tear film following short-term exposure to the Bruder mask.
Thermal pulsation study
In a second study conducted at Matossian Eye, we sought to determine whether thermal pulsation treatment with LipiFlow (Johnson & Johnson Vision) before cataract surgery affects keratometry and surgical decision-making. Twenty-five eyes of 23 subjects with meibomian gland dysfunction (MGD)undergoing cataract surgery were included in the investigation.
At Visit 1, we performed preoperative measurements, including keratometry measured with IOLMaster 700 (Zeiss) and topography measured with the OPD-Scan III (Nidek). Based on these original measurements, the IOL calculations were completed and astigmatism management was planned but set aside for comparison purposes only. We then performed thermal pulsation on these patients.
Six weeks later, at Visit 2, measurements were repeated by the same technician, using the same equipment, and IOL calculations were performed again based on the post-therapy LipiFlow measurements.
There were statistically significant changes in delta K (the difference between flat and steep Ks) and axis of astigmatism between the pre- and post-thermal pulsation sets of measurements. The mean axis change was 22.5±23.9°. The direction of the axis change varied considerably, with about half the axes changing from steep to flat and the others, the reverse. The mean delta K was 0.31±0.20°. It also varied, with an increase in delta K in 16 eyes and a decrease in eight eyes.
Translating this into cataract surgical planning, we found that pre- to post-thermal pulsation treatment keratometry and topography measurements correlated with a 40 percent change from my original surgical plan. Specifically, my surgical plan changed from no intervention to limbal relaxing incision (LRI) or toric in 28 percent of cases. It changed from LRI or toric to no intervention in 8 percent of cases. And my surgical plan changed from a toric to an LRI in 4 percent of cases. Final refractive outcomes were precisely on target in 60 percent of eyes; 88 percent were within ±0.25 D of the intended refraction and 92 percent were within ±0.50 D using the post-therapy LipiFlow measurements.
Pre- and post-op pearls
I perform a complete ocular surface disease workup in 100 percent of my cataract consult patients. Every patient completes a variation of the Standard Patient Evaluation of Eye Dryness (SPEED) questionnaire, and we perform 3 tests on every pre-op candidate: tear osmolarity, MMP-9, and meibography.
The progression to surgery is much faster when ocular surface disease is identified and pretreated by the referring optometrist prior to the first consultation.
If I see ocular surface disease at the time of the cataract consult, I customize treatment based on the severity of the disease and the coexistence of meibomian gland dysfunction (MGD). When MGD is present, I suggest thermal pulsation, a high-quality oral omega fish oil supplement, and a moist heat compress daily. For patients with inflammation, I add a short course of topical steroid drops and discuss the initiation of immunomodulation therapy after cataract surgery as long-term therapy. After 2 to 3 weeks of treatment, I see the patients for their pre-surgical measurements. Even patients who present with a stable tear film on the cataract consultation visit are asked to use preservative-free artificial tears qid for 2 weeks before topography, keratometry, and biometry are performed.
Postoperative ocular surface wellness is essential to maintain the visual results achieved by surgery. It is not uncommon for patients to stop following their chronic dry eye disease treatment routines and return with complaints of fluctuating vision. For this reason, it is important that the MD and OD work together to ensure that the ocular surface remains optimized. To achieve lasting outcomes with this progressive disease, we recommend thermal pulsation once a year, moist heat compresses on a daily basis, and a wide variety of additional prescription, at-home, or in-office treatments depending on disease severity.
References
1. Epitropoulos AT, Matossian C, Berdy GJ, Malhotra RP, Potvin R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015 Aug;41(8):1672-1677.
2. Kim P, Plugfelder S, Slomovic AR. Top 5 pearls to consider when implanting advanced-technology IOLs in patients with ocular surface disease. Int Ophthalmol Clin. 2012 Spring;52(2):51-58.
3. Goldberg DF. Preoperative evaluation of patients before cataract and refractive surgery. Int Ophthalmol Clin. 2011 Spring;51(2):97-107.
4. Ale Magar JB. Comparison of the corneal curvatures obtained from three different keratometers. Nepal J Ophthalmol. 2013 Jan-Jun;5(1):9-15.
5. Manning CA, Kloess PM. Comparison of portable automated keratometry and manual keratometry for IOL calculation. J Cataract Refract Surg. 1997 Oct;23:1213-1216.
6. Willcox MDP, Argüeso P, Georgiev GA, Holopainen JM, Laurie GW, Millar TJ, Papas EB, Rolland JP, Schmidt TA, Stahl U, Suarez T, Subbaraman LN, Uçakhan OO, Jones L. TFOS DEWS II tear film report. Ocul Surf. 2017 Jul;15(3):366-403.
7. Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort. Cornea. 2012 May;31(5):472-478.
8. Tan J, Ho L, Wong K, La A, Lee S, Park S, Tran L, Stapleton F. The effects of a hydrating mask compared to traditional warm compresses on tear film properties in meibomian gland dysfunction. Cont Lens Anterior Eye. 2018 Feb;41(1):83-87.
9. Qiao J, Yan X. Emerging treatment options for meibomian gland dysfunction. Clin Ophthalmol. 2013;7:1797-1803.
10. Knop E, Knop N, Millar T, Obata H, Sullivan DA. The international workshop on meibomian gland dysfunction: report of the subcommittee on anatomy, physiology, and pathophysiology of the meibomian gland. Invest Ophthalmol Vis Sci. 2011 Mar;52(4):1938-1978.
Articles in this issue
over 5 years ago
3 steps to managing scleral lens patients with allergiesover 5 years ago
3 reasons to fit kids with contact lensesover 5 years ago
Dry eye intranasal spray stimulates the trigeminal nervesover 5 years ago
Technology for optometry post COVID-19over 5 years ago
5 essential truths to treating dry eye diseaseover 5 years ago
The evolving standard of care in AMDover 5 years ago
Optimizing ocular blood flow in glaucoma managementover 5 years ago
The time is now for optometry and telehealthover 5 years ago
IPL: The science of comfort and safetyNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.