
- June digital edition 2020
- Volume 12
- Issue 6
Swept-source and multimodal OCT technologies offer clinical advantages
The expenditure of embracing new technologies is worthwhile.
Investing the time, money and resources in new technologies is vitally important, allowing earlier diagnosis, increasing patient confidence and ensuring that decisions are made based on the best data available.
Contemporary optical coherence tomography (OCT) devices are providing clinicians with incredible visual data, reporting tools, and operational benefits. Although “trading up” comes with a considerable (and often intimidating) price tag, in my experience the clinical and business value inherent to these instruments justifies the expenditure.
The modern OCT devices available today—whether those devices offer swept-source (SS) or spectral-domain (SD) imaging technology—are multimodal, meaning clinicians can capture an incredible amount of information both quickly and easily. In one scan, for instance, ODs can observe a patient’s macular thickness, ocular nerve health, retinal nerve fiber layer (RNFL) thickness, cup-to-disc ratio, and more.
Beyond image acquisition, these systems often come equipped with highly sophisticated reporting functions. Software collates key images and data streams in one place, compares results to normative databases (where possible), and, ultimately, allows ODs to make a diagnostic decision with deep and wide data readily available.
The net sum of this functionality is an enhanced ability to quickly and confidently diagnose and monitor posterior segment and glaucomatous disease, as well as other applications in the anterior segment. Here, I’ll review some of the ways we have put modern OCT to work in our practice.
SS imaging benefits posterior segment
Many physicians use OCT to image, diagnose, and monitor posterior segment disease, such as diabetic macular edema (DME), retinal vein occlusion (RVO), and diabetic retinopathy. In this domain, SS-OCT imaging technologies, which scan at higher speeds and use a longer wavelength light source than SD-OCT devices, provide compelling clinical advantages.
The primary advantage of SS-OCT, as evidenced by recent literature and my own clinical experience, is superior visualization of deep anatomical topography, including the choroid. The longer wavelength compared to SD-OCT, combined with the increased signal-to-noise ratio inherent in SS-OCT, better penetrates ocular tissue and challenging media, such as blood and cataracts, to produce high-resolution images of key posterior segment structures. Although contemporary SD-OCT devices remain capable of capturing quality, high-fidelity B-scans, SS-OCT offers consistency across a broader range of anatomical structures.
As an added benefit, Topcon’s DRI OCT Triton swept-source device is capable of capturing 12×9 mm widefield scans, helping us assess both disc and macula in one scan.
OCT and glaucoma diagnosis
Another exciting area in OCT application lies in the realm of glaucoma, in which increasingly sophisticated imaging and reporting tools may facilitate confident, early diagnoses. Multimodal platforms available on the market today can produce a wide range of crucial images and data points, providing information we can use to find abnormalities associated with early glaucomatous disease.
More specifically, practitioners experienced at diagnosing glaucoma can use these systems to (among other applications) quantify circumpapillary RFNL thickness, identify defects of the retinal ganglion cell complex (RGCC), and assess optic nerve health. Clinical research has demonstrated that pathological changes to the RNFL and ganglion cell layer (GCL) in the macula can occur before noticeable changes to the optic nerve head and before identifiable visual field (VF) changes, making early, routine diagnostics workups valuable.3,4
The reporting capabilities offered by the most recent generation of OCT devices are remarkable in both scope and presentation, and these capabilities are especially pertinent in the area of glaucoma, where clinicians must lean on many data points—many of which, as we are learning, are not directly correlative—to make a confident, early diagnosis. The dense data sets enabled by the scanning speed of SS-OCT devices further strengthen this capability. Modern reporting tools collate a large amount of data and compare data to established normative databases in real time, increasing analytical confidence at the point of care.
Case studies
Macular analysis leads to immediate surgical referral
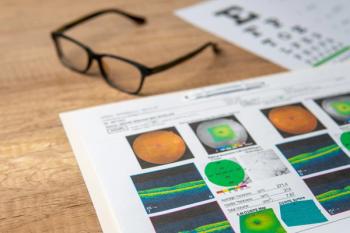
A female patient, age 46, presented with “blurred vision.” Visual acuity OS registered at 20/40-2. Using our swept-source system’s macula report function, we identified a small, full-thickness macular hole (see Figure 1). We immediately referred the patient for a pars plana vitrectomy. Postoperatively, the patient now sees 20/25+2 OS.
Suspected glaucoma revealed as nutritional deficiency
Another 46-year-old female patient presented to our practice without complaint. A fundus exam revealed subtle temporal optic nerve head (ONH) pallor OU. OCTs revealed bilateral temporal RNFL thinning as well as bilateral diffuse macular GCL thinning (characterized by reduced average thickness). The patient’s best-corrected VA was 20/25+2 OD/OS. The patient also exhibited difficulty with color vision testing. No other neurological symptoms were apparent (Figures 2-5).
The patient is a vegetarian and adhering to a low-calorie diet. The patient was sent for blood tests and results indicated severely low vitamin B12 levels, most likely resulting in this optic neuropathy. The patient was immediately placed on weekly intramuscular injections of cyanocobalamin for 5 weeks, then oral B12 and folic acid.
Important patient and practice benefits
Beyond raw imaging power and usability, modern OCT devices provide several advantages in the patient experience and practice development. Chiefly, the fast image acquisition speed inherent to newer devices, especially swept-source devices, reduces patient chair time. In addition to expediency, this is typically more comfortable for patients and also helps reduce the number of “retakes” required in my experience.
Tangentially, we have found that implementing state-of-the-art technology increases patient confidence. The visualization inherent to our SS-OCT device makes patient education easy and engaging, and we find that patients often respond well to our perceived technological savviness. As a practice that emphasizes patient–physician dialogue and constructive consultation, our device has been a boon in this regard.
From a business standpoint, our device’s rapid speed and ease of use allows us to provide comprehensive, high-quality care to more patients in a shorter amount of time. We are able to accelerate a key part of our workflow, meet with more patients, and positively impact our bottom line.
New horizons for imaging technology
As an eyecare professional who is passionate about delivering my patients the best care possible, I view the assessment and integration of new technology as imperative. Although it inevitably costs time and resources to onboard a new OCT system, the value of new iterations cannot be overstated. Even the most experienced clinicians benefit from having deep and wide topographical data at their disposal.
Ultimately, contemporary OCT offers a compelling argument for why clinicians should continue to invest in new and innovative systems as a whole, and imaging devices in particular.
References:
1. Miller AR, Roisman L, Zhang Q, Zheng F, Rafael de Oliveira Dias J, Yehoshua Z, Schaal KB, Feuer W, Gregori G, Chu Z, Chen CL, Kubach S, An L, Stetson PF, Durbin MK, Wang RK, Rosenfeld PJ. Comparison between spectral-domain and swept-source optical coherence tomography angiographic imaging of choroidal neovascularization. Invest Ophthalmol Vis Sci. 2017 Mar;58(3):1499-1505.
2. Qiao Y, Tan C, Zhang M, Sun X, Chen J. Comparison of spectral domain and swept source optical coherence tomography for angle assessment of Chinese elderly subjects. BMC Ophthalmol. 2019;19:42. 142.
3. Liu T, Tatham AJ, Gracitelli CP, Zangwill LM. Weinreb RN, Medeiros FA. Rates of retinal nerve fiber layer loss in contralateral eyes of glaucoma patients with unilateral progression by conventional methods. Ophthalmology 2015 Nov;122(11):2243-2251.
4. Medeiros FA, Zangwill LM, Bowd C, Mansouri K, Weinreb RN. The structure and function relationship in glaucoma: implications for detection of progression and measurement of rates of change. Invest Ophthalmol Vis Sci. 2012 Oct 5;53(11):6939-6946.
Articles in this issue
over 5 years ago
Moncler Lunettes sunglass and eyeglass collection 2020over 5 years ago
Telehealth success hinges on better toolsover 5 years ago
Lactoferrin levels can diagnose dry eye diseaseover 5 years ago
Resolved cotton-wool spot leaves RNFL defect in its wakeover 5 years ago
Patients aren’t hearing contact lens care informationover 5 years ago
11 things my patient wished her previous OD had told herover 5 years ago
Proper documentation helps assure prior authorizationsover 5 years ago
What a practice owner would advise her younger selfover 5 years ago
OCT, OCTA show promise in screening for DRNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.












































.png)


