Aflibercept PANORAMA study results in
Patients who switched to as-needed dosing experienced increased complications
Two-year results from the PANORAMA study show steady improvement with aflibercept injections in moderately severe to severe nonproliferative diabetic retinopathy. Less improvement was seen in those patients who switched to as-needed dosing in Year 2 suggesting that a defined-treatment interval regimen may result in better outcomes, whereas a PRN regimen may lead to under-treatment in some cases due to inaccurate clinical grading of NPDR severity by retina specialists.
Mounting evidence shows that earlier intervention with intravitreal anti- Vascular endothelial growth factor (VEGF) therapy (AVT) in patients with non-proliferative diabetic retinopathy (NPDR) often results in significant regression of NPDR severity.
Specifically, both ranibizumab (Lucentis, Genentech) and aflibercept (Eylea, Regeneron) have been shown to induce at least a 2-step improvement in Diabetic Retinopathy Severity Scale (DRSS) in more than 35 percent of subjects being treated for center-involved diabetic macular edema (CI-DME) with anti-VEGF therapy, an effect that was most pronounced for those with DRSS Level 47 (moderately severe) or Level 53 (severe) NPDR at baseline.1,2
Phase 3 PANORAMA study
PANORAMA is a randomized, multi-center, placebo-controlled Phase 3 clinical trial enrolling 402 patients with DRSS Level 47 or 53 NPDR only. It was designed as the first prospective study to test the hypothesis that AVT also can induce NPDR regression as well as prevent worsening disease in patients having moderately severe or severe NPDR without DME.
The primary objective was to determine the proportion of subjects to achieve at least a 2-step reduction in DRSS with 2 different dosing intervals of aflibercept (injections every 8 weeks after 5, monthly loading dose injections or every 16 weeks after 3, monthly loading dose injections) compared with placebo injections at the same interval.3
A secondary outcome of PANORAMA is the percentage of subjects in each group progressing to the development of either a “vision-threatening complication” (VTC)—defined as proliferative diabetic retinopathy (PDR) and/or anterior segment neovascularization (ASNV)—and/or future CI-DME, the leading cause of vision loss in diabetes.4Subjects in the 3 arms were well matched for diabetes duration (about 15 years), HbA1c (about 8.5 percent), gender (about 55 percent male), and diabetes sub-type (90+ percent with type 2 diabetes.)
At 52 weeks, 65 percent and 80 percent of aflibercept subjects achieved ≥2-step DRSS improvement in the Q16 and Q8 week arms, respectively, compared to 15 percent of the observational group (p<0.001 vs sham). Treatment also reduced the chance of developing VTC by 82 percent/85 percent and CI-DME by 74 percent/68 percent in the Q16 and Q8 week arms, respectively (p<0.003 vs sham).
Although a secondary outcome, this risk reduction translates to a number needed to treat (NNT) of only 3 patients to prevent 1 case of PDR/ASNV or CI-DME. This low NNT value is extremely favorable when compared to common therapies like 1 year of daily aspirin use to prevent 1 primary non-fatal heart attack (NNT=2000) or even 5 years of statin therapy to prevent 1 cardiovascular death in patients with known heart disease (NNT=83).5,6
PANORAMA 100-week study results
The results from PANORAMA Week 100 were recently virtually presented at the Angiogenesis, Exudation and Degeneration conference.7 Subjects who continued aflibercept therapy every 16 weeks maintained a consistent 62 percent rate of ≥2-step DRSS improvement compared to baseline, whereas subjects who received Q8 week injections in Year 1 and were switched to PRN injections in Year 2 did less well, with 50 percent achieving ≥2-step improvement versus baseline, down from 80 percent at Year 1.
Rates of VTC and/or CI-DME remained significantly lower in both treatment groups compared to sham (79 percent and 75 percent reduced risk for Q16 week and Q8 week to PRN groups, respectively; p<0.0001).
Why did the Q8 week to PRN group do less well on step improvements than the consistent Q16 week group at the end of 100 weeks? In brief, under-grading of diabetic retinopathy severity by treating retina specialists compared to image reading center grading resulted in under-treatment in Year 2. (From 52 to 100 weeks, roughly 30 percent of eyes were graded as being less severe by retina specialists compared to the reading center, and the mean number of injections was 3 versus 1.8 in the Q16 versus Q8 to PRN groups, respectively).
Application
This is very important for optometrists to understand: Even retina specialists often under-grade NPDR severity and under-treat clinical trial subjects per PANORAMA protocol criteria calling for additional aflibercept therapy in the Q8 week to PRN arm if DRSS was ≥Level 43 at follow-up.
This finding suggests that defined-interval therapy (e.g., injections every 8 weeks for the first 6 to 12 months followed by Q16 weeks from that time forward) may result in better outcomes than relying on retina specialists’ individual clinical assessments of patients being treated to prevent worsening NPDR and vision-threatening complications.
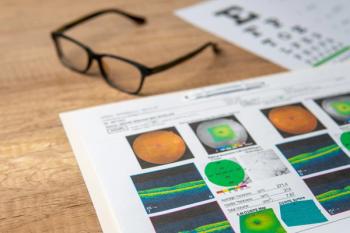
This also underscores consideration of earlier referral of NPDR patients to retina specialists for more definitive diagnostic testing (e.g. ultra-widefield fluorescein angiography; UWF-FA) when ODs detect and grade NPDR of moderate or worse severity (author’s opinion). Figure 1 illustrates a patient with diabetes with relatively limited retinal findings who was found to have more significant disease with UWF-FA.
It is important for ODs to understand that careful observation (“watchful waiting”) has been the standard approach to managing these moderately severe to severe NPDR patients until such time that they develop PDR and/or CI-DME. In total, clinical trials evaluating DR improvement in these patients, both with and without DME, demonstrate significant benefit for patients who previously would have been counseled only on improved metabolic care without pharmacologic intervention, and set the stage for ODs to talk about evidence-based treatment with retina specialists to whom we refer.
References
1. Wykoff CC, Eichenbaum DA, Roth DB, Hill L, Fung AE, Haskova Z. et al. Ranibizumab Induces Regression of Diabetic Retinopathy in Most Patients at High Risk of Progression to Proliferative Diabetic Retinopathy. Ophthalmol Retina. 2018 Oct;2(10):997-1009.
2. Dhoot DS, Baker K, Saroj N, Vitti R, Berliner AJ, Metzig C, Thompson D, Singh RP. et al. Baseline Factors Affecting Changes in Diabetic Retinopathy Severity Scale Score After Intravitreal Aflibercept or Laser for Diabetic Macular Edema: Post Hoc Analyses from VISTA and VIVID. Ophthalmology. 2018 Jan;125(1):51-56
3. ClinicalTrials.gov. Study of the Efficacy and Safety of Intravitreal (IVT) Aflibercept for the Improvement of Moderately Severe to Severe Nonproliferative Diabetic Retinopathy (NPDR) (PANORAMA). Available at: https://clinicaltrials.gov/ct2/show/NCT02718326. Accessed 5/16/20.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.