Role of comorbidities in management of diabetic retinopathy
ODs must pay close attention and manage all factors responsible for disease progression to improve the patient’s final outcome. The patient in this case report shows the importance of such management.
Beyond duration of the disease and status of the blood sugar control, other factors tat negatively influence the prognostic outcomes of patients with diabetic retinopathy.
Modifiable factors include:
• Patient’s poor compliance with follow-up care
• Tobacco use
• Sedentary lifestyle
• Obesity
Systemic comorbidities include;
• Hypertension
• Hyperlipidemia
• Sleep apnea
• Renal disease
• Autoimmune disease
• Blood dyscrasias, often overlooked
Case report
The case summarized here is that of a 47-year-old African-American female. At the time of her initial presentation, she had been diagnosed with poorly controlled type 2 diabetes and hypertension for approximately 15 years. She was on dialysis as well and was sporadically treated for anemia.
The patient was initially diagnosed with proliferative diabetic retinopathy and underwent a series of treatments including intravitreal anti-vascular endothelial growth factor (VEGF) injections (IVI) and panretinal photocoagulation (PRP).
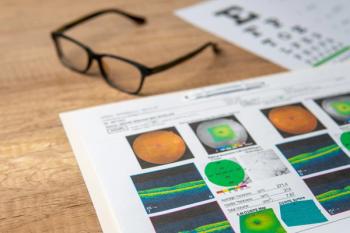
The retinopathy was subsiding, as shown in Figure 1, and the patient was asked to follow up in 2 months; she failed to appear.
Nearly 6 months later, she presents with a complaint seeing sudden onset floaters in the right eye. As evident in Figure 2, the patient’s symptoms were caused by a vitreous hemorrhage in the right eye, and a worsening of the retinopathy was noted in both eyes. Clinically, the observation of multiple deep vascular plexus retinal hemorrhages (also referred to as blot hemorrhages, as well as a number of white-centered hemorrhages (also called
Clinicians also need to keep in mind the anemia, which is a complication of chronic kidney disease.
The patient was treated with anti-VEGF IVI in both eyes. The findings and concern with her blood count were communicated to her primary-care physician (PCP).
At the patient’s one-month follow-up visit, significant resolution of retinal hemorrhages was noted (Figure 4). The patient also indicated receiving additional iron therapy from her PCP.
ODs must pay close attention and manage all factors responsible for disease progression to improve the patient’s final outcome.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.