Case report: OCT in the detection and diagnosis of neurofibromatosis type 1
Neurofibromatosis type 1 (NF1) is a condition associated with significant systemic morbidity. Abnormal proliferation of cells derived from the neural crest can cause benign and malignant tumors throughout the body in NF1.
NF is a systemic condition characterized by the abnormal proliferation of cells derived from the neural crest.1,2 This can lead to various malignancies including malignant schwannoma, rhabdomyosarcoma, nephroblastoma, myelogenous leukemia, and melanoma.2 (Image credit: Adobe Stock/NDABCREATIVITY)

Neurofibromatosis type 1 (NF1) is a condition associated with significant systemic morbidity. Abnormal proliferation of cells derived from the neural crest can cause benign and malignant tumors throughout the body in NF1.1,2 Early diagnosis and close monitoring are essential in the management of this disease, and ocular manifestations may be the first detected sign.
Historically, iris Lisch nodules have been the primary ocular manifestation used in the diagnosis of NF1.3,4 With the advent of newer technologies, it is possible to obtain highly detailed images of the choroid, and recent research data have shown that choroidal nodules are equally as common as or perhaps more common than Lisch nodules in NF1.1,5-7 Retinal and choroidal lesions were previously considered rare but are now included in proposed updated diagnostic criteria. According to these criteria, the diagnosis of NF1 can be made with the detection of 2 or more choroidal abnormalities and a parent with a confirmed diagnosis of NF1.3 The following case report describes incidental choroidal findings on optical coherence tomography (OCT) imaging that prompted the diagnosis of NF1.
Case report
A 25-year-old woman presented for a comprehensive eye examination complaining of eye strain and eye fatigue. She noted that her symptoms improved with glasses wear. Additionally, she complained of occasional headaches associated with studying and long hours of computer work. She reported that her headaches resolved with rest and occasional use of over-the-counter pain relievers. She denied symptoms of tinnitus or visual obscuration. Her medical history was unremarkable.
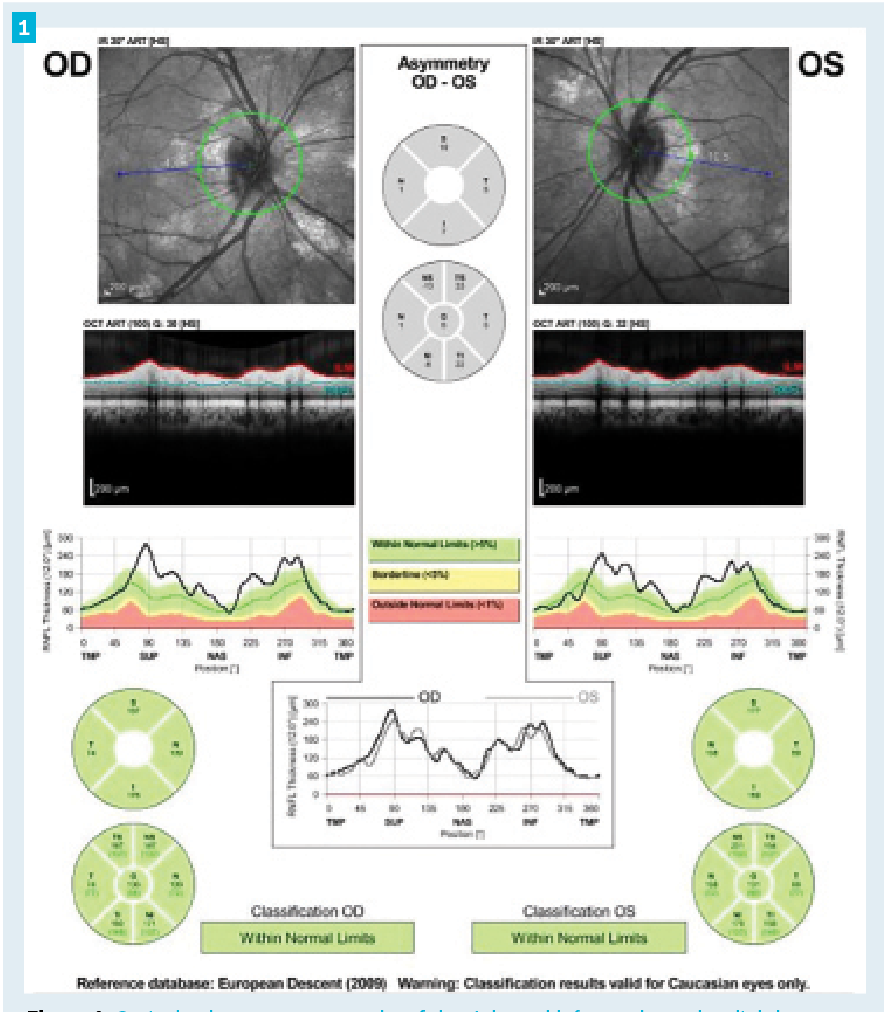
Figure 1. Optical coherence tomography of the right and left eye showed a slightly thickened retinal nerve fiber layer in each eye. Of note, infrared imaging revealed multiple bright chorodial lesions surrounding the opic nerve in each eye.
Best corrected visual acuity was 20/20 in each eye with mild hyperopic astigmatism in each eye. Her pupils were equal, round, and reactive to light with no relative afferent pupillary defect in either eye. Confrontation visual fields were full to finger counting in each eye. Extraocular motilities were full. A cover test showed orthophoria at distance and a small angle exophoria at near. Color vision with Ishihara test plates was full in each eye, showing no color vision deficit in either eye. Anterior segment examination revealed 2 small tan iris lesions in the right eye and no remarkable findings in the left eye. A review of previous eye exam records revealed that these iris lesions had been noted 7 years prior without further comment. IOP was measured to be 15 mmHg in the right eye and 14 mmHg in the left eye using an iCare tonometer.
A dilated posterior segment examination revealed small optic nerves with a cup to disc ratio of 0.1 in each eye. The optic nerve borders appeared slightly elevated and blurred in both eyes. No spontaneous venous pulsation was noted in either eye. The retina appeared normal in each eye with flat maculas and positive foveal light reflexes, normal vessel caliber, and no other remarkable findings.
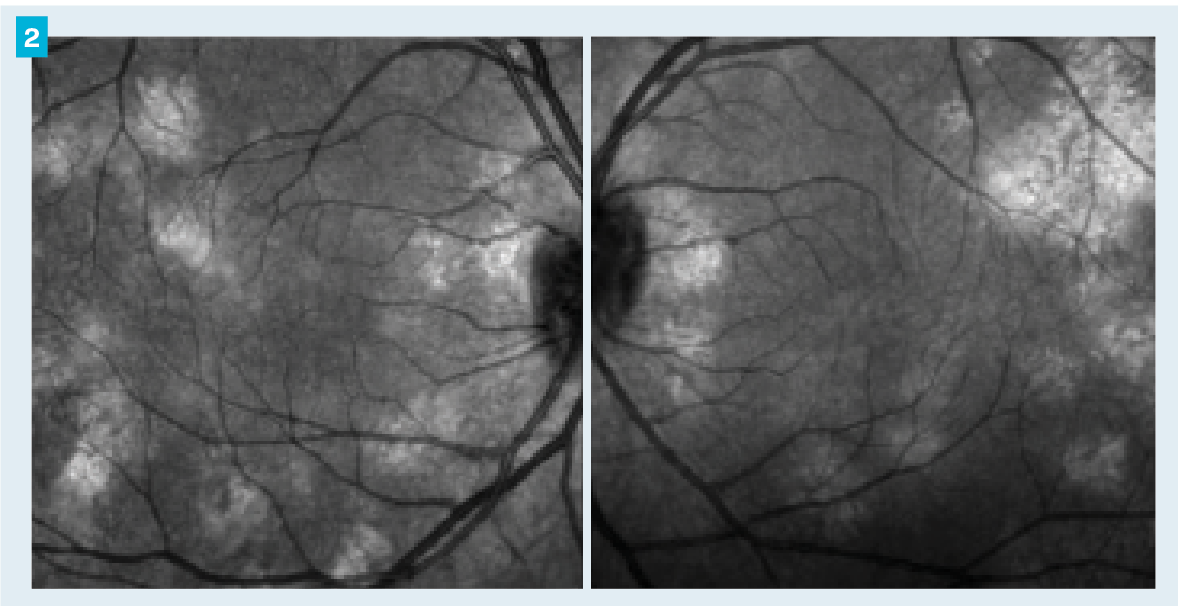
Figure 2. Infrared images on optical coherence tomography showed multiple bright choroidal lesions throughout the posterior pole of each eye.
The patient’s headache symptoms and optic nerve appearance raised suspicion for optic nerve edema. OCT and visual field testing were performed.
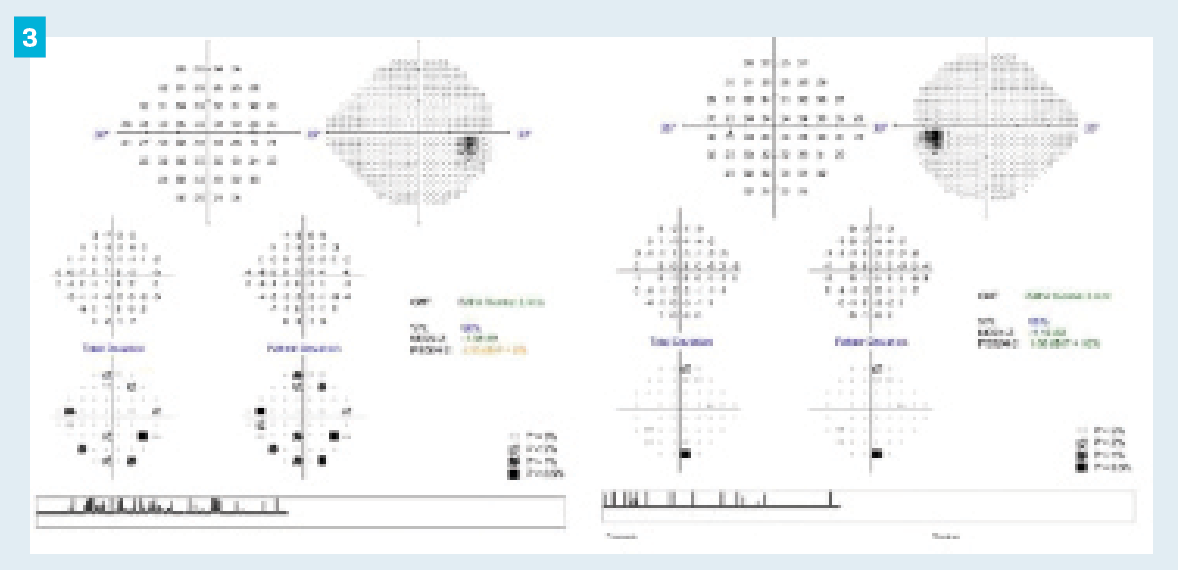
The OCT showed slight thickening of the retinal nerve fiber layer in each eye (Figure 1). Additionally, infrared images showed multiple bright choroidal lesions throughout the posterior pole in both eyes (Figure 2). Humphrey visual field testing showed no significant defects in either eye (Figure 3).
Figure 3.Humphrey visual field testing (24-2 Swedish Interactive Thresholding Algorithm Standard) revealed no significant defects in either eye.
On further questioning, the patient reported that her mother had a known diagnosis of NF1. An MRI was ordered and the patient was referred to the neuro-ophthalmology department for evaluation. The MRI of the brain and orbits showed no optic nerve enhancement or edema, and importantly it showed no signs of optic pathway gliomas associated with NF1. Due to ongoing suspicion of mild optic nerve edema, the neuro-ophthalmology provider ordered a lumbar puncture and CSF analysis. Opening pressure was normal and CSF composition was unremarkable. It was documented that the retinal nerve fiber layer thickening may truly be an incidental finding and annual monitoring was recommended.
Discussion
NF is a systemic condition characterized by the abnormal proliferation of cells derived from the neural crest.1,2 This can lead to various malignancies including malignant schwannoma, rhabdomyosarcoma, nephroblastoma, myelogenous leukemia, and melanoma.2 Because of the possibility of significant morbidity and mortality, early diagnosis and frequent monitoring is essential. Diagnosis of NF is made clinically using certain defining features of the disease.4 Traditionally, 2 or more of the following are required for diagnosis: 6 or more café au lait spots, axillary or inguinal freckling, 2 or more cutaneous neurofibromas, 1 plexiform neurofibroma, distinctive osseous lesions (eg, pseudarthrosis, sphenoid wing hypoplasia), optic glioma, 2 or more iris Lisch nodules, and a first-degree relative with NF1.8
In the past, iris Lisch nodules were the most common ocular feature reported in the literature.3.4 Retinal and choroidal lesions associated with NF1 have historically been reported as rare.1,9 With the advent of newer imaging technologies, detailed imaging of the retina and choroid has become easier and more accessible. A routine OCT image often includes an infrared image of the optic nerve and posterior pole. Near-infrared reflectance (NIR) images the choroid well and in NF1 frequently shows patchy bright lesions in the choroid.5-7,10 These lesions are believed to be a proliferation of neoplastic Schwann cells and are most frequently documented within the posterior pole.1,5-7 Choroidal nodules are not detected on conventional ophthalmoscopic evaluation or fluorescein angiography.1,9 Indocyanine green angiography (ICGA) is another modality which images the choroid well and these lesions show hypofluorescence on ICGA.1,10 However, ICGA is an invasive test and is not commonly performed in all practice settings. The frequency of choroidal nodules in NF1 has been shown to be equal to, if not more common than, that of Lisch nodules.1,5-7 This is especially true in pediatric populations in which Lisch nodules may not be present at young ages.5,7 In addition to frequency, these lesions are highly specific to NF1 and are rarely, if ever, seen in control patients or those with other café-au-lait syndromes such as Legius syndrome.3,5,6
Because of the documented high frequency, sensitivity, and specificity of choroidal nodules in NF1, a new proposed diagnostic criteria includes both Lisch nodules and choroidal abnormalities. In the updated criteria, ocular findings can include 2 or more Lisch nodules or 2 or more choroidal abnormalities––defined as bright patchy nodules imaged by OCT/NIR imaging.3
In this case, 2 small iris lesions were noted at a previous eye exam without further investigation or comment. This may have been because the finding was unilateral; this is rare in NF, in which 93% of Lisch nodules are reported to be bilateral.4 Iris lesions can also be mistaken for nevi, normal color variations, or granulomas, or can simply go undetected in a routine exam. The true turning point of this case was the incidental finding of choroidal lesions on infrared imaging. Using updated diagnostic criteria, the diagnosis of NF1 could be made based on the presence of 2 or more choroidal abnormalities and a parent with confirmed NF1.
As eye care providers, we can find ourselves at the forefront of the detection and diagnosis of systemic disease. New technologies improve our ability to do so and to provide more comprehensive care to our patients.
References
1. Yasunari T, Shiraki K, Hattori H, Miki T. Frequency of choroidal abnormalities in neurofibromatosis type 1. Lancet. 2000;356(9234):988-992. doi:10.1016/S0140-6736(00)02716-1
2. To KW, Rabinowitz SM, Friedman AH, Merker C, Cavanaugh CP. Neurofibromatosis and neural crest neoplasms: primary acquired melanosis and malignant melanoma of the conjunctiva. Surv Ophthalmol. 1989;33(5):373-379. doi:10.1016/0039-6257(89)90014-3
3. Legius E, Messiaen L, Wolkenstein P, et al. Revised diagnostic criteria for neurofibromatosis type 1 and Legius syndrome: an international consensus recommendation. Genet Med. 2021;23(8):1506-1513. doi:10.1038/s41436-021-01170-5
4. Huson S, Jones D, Beck L. Ophthalmic manifestations of neurofibromatosis. Br J Ophthalmol. 1987;71(3):235-238. doi:10.1136/bjo.71.3.235
5. Viola F, Villani E, Natacci F, et al. Choroidal abnormalities detected by near-infrared reflectance imaging as a new diagnostic criterion for neurofibromatosis 1. Ophthalmology. 2012;119(2):369-375. doi:10.1016/j.ophtha.2011.07.046
6. Cassiman C, Casteels I, Jacob J, et al. Choroidal abnormalities in café-au-lait syndromes: a new differential diagnostic tool? Clin Genet. 2017;91(4):529-535. doi:10.1111/cge.12873
7. Vagge A, Camicione P, Capris C, et al. Choroidal abnormalities in neurofibromatosis type 1 detected by near-infrared reflectance imaging in paediatric population. Acta Ophthalmol. 2015;93(8):e667-e671. doi:10.1111/aos.12750
8. Neurofibromatosis: conference statement: National Institutes of Health Consensus Development Conference. Arch Neurol. 1988;45(5):575-578.
9. Ishiko S, Yoshida A, Kato Y, Kagokawa H. Occult retinal and choroidal lesions in neurofibromatosis type 1. Br J Ophthalmol. 2006;90(8):1067-1068. doi:10.1136/bjo.2006.092718
10. Kumar V, Singh S. Multimodal imaging of choroidal nodules in neurofibromatosis type-1. Indian J Ophthalmol. 2018;66(4):586-588. doi:10.4103/ijo.IJO_1095_17
