- December digital edition 2020
- Volume 12
- Issue 12
Cataract surgery 2020 update
Find out the latest on technologies, techniques, and treatments
Cataract surgery is evolving at a rapid pace. Given that optometrists are the primary eyecare providers for most patients, it is essential that they understand the advances in cataract surgery techniques and treatments. Being well informed enables ODs to counsel patients and serve as a trusted source of information as patients prepare for cataract surgery. It can also lead to better outcomes because ODs can share with surgeons their knowledge of patients’ history, visual needs, and expectations.
The optometrist’s role in surgical comanagement will only continue to grow. Current projections show that by 2025 in the United States there will be a deficit of ophthalmologists.1 However, an aging population will lead to increased demand for vision care and specifically preoperative and postoperative care of surgical procedures. Optometrists will be called upon to close that supply and demand gap.
In recent years, there have been improvements in dry eye care, cataract surgical technology, intraocular lenses (IOL), and the prevention of post-surgical pain and inflammation, all ultimately aimed at improving outcomes and the patient experience.
Addressing ocular surface disease
One of the most important steps that optometrists can take to prepare their patients for cataract surgery is to screen for and treat ocular surface disease, dry eye, and meibomian gland dysfunction (MGD).
In our practice, patients complete a symptom questionnaire and, if warranted, point-of-care testing and further dry eye workup, including ocular surface staining and meibography.
In a recent study of 120 cataract surgery patients, 80 percent had at least one abnormal tear test suggestive of ocular surface dysfunction, and 40 percent had two abnormal results.2 Treating the signs and symptoms of ocular surface disease prior to surgery is essential to ensuring accurate IOL power calculations, successful refractive outcomes, and high patient satisfaction.
Surgical technologies
New intraoperative tools may make surgery faster, easier, and/or reduce the chance of complications. Use of these technologies can serve as an indicator that the surgeons ODs partner with are investing in cutting-edge technology for their patients. For example, a major innovation with femtosecond laser-assisted cataract surgery (FLACS), which was first approved 10 years ago, was the automation of the capsulotomy, providing greater consistency in IOL centration, which can impact the final lens position and tilt.
Since then, other approaches to anterior capsulotomy creation have been developed. The Zepto (Mynosys) precision pulse capsulotomy device consists of a nanoengineered circular nitinol ring with a superelastic shape memory alloy that enables it to enter through a small clear corneal incision and resume its circular shape once in the anterior chamber; a brief (4 ms) series of electrical pulses is emitted from the ring, creating a perfectly round capsulotomy.3
The CAPSULaser (Excel-Lens), or selective laser capsulotomy, utilizes a non-contact laser to deliver a continuous pulse of thermal energy, creating a circular capsulotomy in one second. Still in development, its benefits may include efficiency and a more stable, stronger anterior capsule compared to manual capsulorrhexis and FLACS. The Aperture CTC (International Biomedical Devices), or continuous thermal capsulotomy (CTC), is in pre-clinical testing and delivers thermal energy that melts the collagen of the anterior capsule and is capable of creating a 4.5 to 6.5 mm capsulotomy.4
New intraoperative measurement and visualization tools have also helped to refine cataract surgery. For example, intraoperative aberrometry (Optiwave Refractive Analysis, Alcon) gives surgeons more accurate information on lens power and placement, aids in aligning toric IOLs, and helps surgeons compensate for surgically induced astigmatism and posterior corneal curvature. In a U.S. study of 130 patients (260 eyes), 89 percent of astigmatic eyes in the intraoperative aberrometry group measured 0.50 D or less from their target refraction at 1 month as compared to 77 percent in the control group.5
Making its way from retinal procedures into cataract surgery is 3D visualization, a technology that provides a “heads up” view of the eye during cataract surgery, without the necessity for individual microscopic viewing. This technology (NGENUITY 3D, Alcon) allows the ability to observe the anterior chamber with an extended depth of field, maintains the surgeon’s posture and has the potential to be utilized for cataract surgery and minimally invasive glaucoma surgeries.6
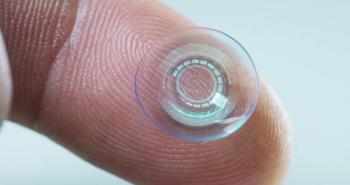
Intraocular lenses
Significant advances are occurring in the IOL space, giving patients new options to reduce their dependence on spectacles or contact lenses after cataract surgery. Setting proper expectations, proactively treating the ocular surface, picking the right IOL for the patient, and properly screening patients for other ocular diseases are essential for the success of presbyopia-correcting IOLs.
While traditional presbyopia-correcting IOLs are designed primarily for better distance and close vision, more recent lenses are designed for better close, distance, and intermediate vision. For example, the recent U.S. Food & Drug Administration approved, AcrySof IQ PanOptix IOL (Alcon) offers 3 focal points: near at 40 cm, intermediate at 60 cm, and infinity.7 PanOptix was designed with a 4.5-mm diffractive zone, making it less dependent on pupil size than other presbyopia-correcting IOLs.7
In contrast to a monovision approach with a monofocal IOL, or a mix-and-match approach with multifocal IOLs, binocular summation is not compromised in patients who receive PanOptix bilaterally. The lens comes in a toric design as well, allowing it to correct corneal astigmatism.
Following the procedure, it is important to inform patients that they may notice glare in the presence of bright lights and halos, especially at night.7 I always tell my patients this lens is intended to reduce dependence on glasses, not to completely eliminate them, and allows good distance, intermediate, and near vision. A patient survey component of the U.S. Food & Drug Administration (FDA) clinical study revealed that 99 percent of patients who received PanOptix said they would choose this lens again.8
Another innovation is provided by the extended range of vision IOLs, which includes the Tecnis Symfony (Johnson & Johnson Vision; Figure 1).
This technology uses a proprietary design of 9 echelettes that are taller than those on the multifocal IOL and are slightly angled. This pattern of light diffraction elongates the focus resulting in an increased depth of focus, thereby enhancing near and intermediate vision without compromising distance vision. Using diffractive optics, it reduces chromatic aberration, extends the range of vision to approximately 1.50 D, and retains contrast sensitivity similar to the level of monofocal IOLs.9
Next-generation modified monfocal IOLs is another category that will attempt to fill a niche to provide patients concerned about positive dysphotopsias or other eye-related concerns that may prevent the use of a multifocal/trifocal IOL. Two implants, AcrySof IQ Vivity and Tecnis Eyhance, proved an extended range of vision, less than a multifocal IOL, but with the hope of less positive dysphotopsias and high contrast sensitivity under a variety of lighting conditions.
The Light Adjustable Lens (LAL) system is a novel IOL technology used to correct residual refractive error and improve uncorrected visual acuity after cataract surgery. About 17 days post-implantation, a Light Delivery Device is used to adjust the implant to correctresidual refractive error, including residual astigmatism (Figure 2). Up to 3 adjustments may be made before 1 or 2 lock-in procedures occurs to reach the ultimate lens power.
In the FDA clinical trial, 92 percent of patients who received the LAL achieved 20/25 or better, while 90 percent of those in the control group achieved only 20/40 or better. Additionally, 92 percent of those who received the LAL achieved a result within 0.50 D of target. It is important to inform patients that they will need to wear UV-protecting glasses both inside and outside until the LAL is locked in.10
Many IOL technologies on the horizon will continue to help improve and evolve the space. Modular IOL systems that allow placement of a base in the capsular bag and a removable optic will allow predictable outcomes from the start, along with the flexibility to exchange the optic at any time. Multiple accommodating IOL technologies and new extended depth-of-focus IOLs aim to decrease the glare and halo challenges that plague some patients with other IOL technologies. Finally, a new “pinhole” or small-aperture design placed in the nondominant eye allows for increased depth of focus to provide some near visual acuity with continued adequate distance visual acuity.
New drug formulations
ODs know that patients face a number of challenges with post-cataract surgery eye drop regimens. For example, drop administration triggers immediate increases in tear volume and rapid reflex blinking, substantially limiting residence time on the ocular surface and the ability for active drug to penetrate into intraocular tissues.11,12
Additionally, many drops do not even make it to the ocular surface because patients may apply them incorrectly or forget to apply them at all. The consequences of poor adherence to drop regimens range from discomfort and delayed visual recovery to an increased risk of serious complications like infection and central macular edema. A number of newer entrants to the field of post-cataract anti-inflammatories have been developed to circumvent some of these obstacles.
Compared with prior formulations of loteprednol etabonate, the drug particle size in Lotemax SM (loteprednol etabonate ophthalmic gel 0.38%; Bausch + Lomb) has been reduced to 0.4 to 0.6 µm, enabling faster dissolution and ocular penetration.13,14 The polycarbophil gel matrix, coupled with the smaller particle size, allows Lotemax SM to cover a larger surface area and exposes it to more tear film. As the drug dissolves, there is a higher concentration in the tears, allowing more medication to penetrate the ocular tissues.
New drug delivery technologies reduce the need for patient administration postoperatively, making them more convenient for patients. For example, Dexycu (dexamethasone intraocular suspension 9%; EyePoint) is a sustained-release drug-delivery suspension indicated for the treatment of postoperative inflammation and administered into the posterior chamber behind the iris at the conclusion of ocular surgery.15 ODs should know that Dexycu can migrate and be visible as a white sphere in the anterior chamber (Figure 3). As the active ingredient is released, the sphere becomes less noticeable as it biodegrades and eventually disappears.
In a Phase 3 trial among patients undergoing cataract surgery, significantly more eyes treated with Dexycu had clearance of anterior chamber cells at postoperative Day 8 (66 percent vs 25 percent for placebo/vehicle, P<0.001).16 Dexycu was also compared in an open-label safety study to prednisolone acetate 1% (qid for 3 weeks) and was found to have equivalent safety, including IOP response and corneal endothelial cell count, and efficacy, to the topical comparator.17
Dextenza (dexamethasone insert 0.4 mg; Ocular Therapeutix) is an intracanalicular insert consisting of a polyethylene glycol (PEG)-based hydrogel depot that allows for sustained and tapered release of dexamethasone to the ocular surface for up to 30 days.18 The insert is FDA approved for the treatment of inflammation and pain following ophthalmic surgery. The punctum is dilated for quick insertion of the device, which expands rapidly as it interacts with the tear fluid. The insert resorbs over time and eventually exits through the nasolacrimal duct without the need for removal; it is impregnated with fluorescein to enable visualization at the slit lamp, using a cobalt blue light.19
In addition to these FDA-approved medications, compounded topical and intraocular formulations are used by some surgeons to help address the challenge of patient adherence to postoperative drops. Some topical compounded formulations combine a steroid, antibiotic, and non-steroidal anti-inflammatory drug (NSAID) in one bottle, which substantially increases convenience for the patient, and may reduce the cost significantly. The administration of intracameral antibiotic during cataract surgery is increasingly common, despite the lack of a commercially available formulation. Multiple studies have shown that this approach reduces the risk for endophthalmitis.20,21
Conclusion
This is an exciting time in the evolution of cataract surgery, with many new options that increase patients’ comfort and convenience and provide the visual quality and range of vision that patients desire after cataract surgery. ODs provide patients with a great service by preparing them adequately for surgery, choosing surgical referral partners who have adopted new technologies, and helping to educate patients about what to expect.
References
1. U.S. Department of Health and Human Services. Health Resources and Services Administration. Bureau of Health Workforce. National Center for Health Workforce Analysis. National and Regional Projections of Supply and Demand for Surgical Specialty Practitioners. 2013-2025. December 2016. Available at: https://bhw.hrsa.gov/sites/default/files/bhw/health-workforce-analysis/research/projections/womens-health-report.pdf. Accessed 11/20.20.
2. Gupta PK, Drinkwater OJ, et al. Prevalence of ocular surface dysfunction in patients presenting for cataract surgery evaluation. J Cataract Refr Surg. 2018 Sep;44(9):1090-1096.
3. Chang DF. Zepto precision pulse capsulotomy: A new automated and disposable capsulotomy technology. Indian J Ophthalmol. 2017 Dec;65(12):1411-1414.
4. American Academy of Ophthalmology EyeWiki. Automated Capsulotomy Devices. Available at: https://eyewiki.aao.org/Automated_Capsulotomy_Devices. Accessed 11/22/20.
5. Woodcock MG, Lehmann R, Cionni RJ, Breen M, Scott MC. Intraoperative aberrometry versus standard preoperative biometry and a toric IOL calculator for bilateral toric IOL implantation with a femtosecond laser: One-month results. J Cataract Refract Surg. 2016 Jun;42(6):817-825.
6. Ohno H. Utility of Three-Dimensional Heads-Up Surgery in Cataract and Minimally Invasive Gluacoma Surgeries.Clin Ophthalmol.2019 Oct;13: 2071-2073.
7. Sudhir RR, Dey A, Bhattacharrya S, Bahulayan A. AcrySof IQ PanOptix intraocular lens versus extended depth of focus intraocular lens and trifocal intraocular lens: a clinical overview. Asia Pac J Ophthalmol (Phila). 2019 Jul-Aug;8(4):335-349.
8. Food & Drug Administration. Summary of Safety and Effectiveness Data (SSED) for AcrySof PanOptix Trifocal Intraocular Lens (Model TFNT00) and AcrySof PanOptix Toric Trifocal Intraocular Lens (Model TFNT30, TFNT40, TFNT50, TFNT60). Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf4/P040020S087B.pdf. Accessed 11/22/20.
9. Rocha KM. A Unique Optical Design. Clinical and Practical Considerations for Extended Depth of Focus IOLs. Rev Ophthalmol. Available at: https://www.reviewofophthalmology.com/CMSDocuments/2017/05/AMO_SHEDDi.pdf. Accessed 11/24/20.
10. Food & Drug Administration. Summary of Safety and Effectiveness Data (SSED) for Light Adjustable Lens (LAL)/Light Delivery Device (LDD). Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf16/P160055B.pdf. Accessed 11/22/20.
11. Ghate D, Edelhauer H. Ocular drug delivery. Expert Opin Drug Deliv. 2006 Mar;3(2):275-287.
12. Guadana R, Ananthula HK, Parenky A, Mitra AK. Ocular drug delivery. AAPS J. 2010 Sep;12(3):348-360.
13. Bausch + Lomb. Lotemax SM (loteprednol etabonate ophthalmic gel) [package insert]. Available at: https://www.bausch.com/Portals/69/-/m/BL/United%20States/USFiles/Package%20Inserts/Pharma/lotemax-sm-package-insert.pdf. Accessed 11/22/20.
14. Cavet ME, Glogowski S, Lowe ER, Phillips E. Rheological Properties, dissolution kinetics, and ocular pharmacokinetics of loteprednol etabonate (submicron) ophthalmic gel 0.38%. J Ocul Pharmacol Ther. 2019 Jun;35(5):291-300.
15. Icon Bioscience. Dexycu (dexamethasone intraocular suspension) [package insert]. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/208912s000lbl.pdf. Accessed 11/22/20.
16. Donnenfeld E, Holland E. Dexamethasone intracameral drug-delivery suspension for inflammation associated with cataract surgery: a randomized, placebo-controlled, phase III trial. Ophthalmology. 2018 Jun;125(6):799-806.
17. Donnenfeld ED, Solomon KD, Matossian C. Safety of IBI-10090 for inflammation associated with cataract surgery: Phase 3 multicenter study. J Catract Refract Surg. 2018 Oct;44(10):1236-46.
18. Ocular Therapeutix, Inc. Dextenza (dexamethasone ophthalmic insert) [package insert]. Available at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/208742s001lbl.pdf. Accessed 11/22/20.
19. Walters T, Bafna S, Vold S, Wortz G, Harton P, Levenson J, Hovanesian J, Mah F, Gira J, Vroman D, Sampson R, Berdahl J, Elmer T, Noecker RJ. Efficacy and safety of sustained release dexamethasone for the treatment of ocular pain and inflammation after cataract surgery: results from two phase 3 studies. J Clin Exp Ophthalomol. 2016;7(4):572-583.
20. George NK, Stewart MW. The routine use of intracameral antibiotics to prevent endophthalmitis after cataract surgery: How good is the evidence? Ophthalmol Ther. 2018 Dec;7(2):233-245.
21. Shorstein NH, Winthrop KL, Herrinton LJ. Decreased postoperative endophthalmitis rate after institution of intracameral antibiotics in a Northern California eye department. J Cataract Refract Surg. 2013 Jan;39(1):8-14.
Articles in this issue
about 5 years ago
New ways to keep dry eye patients comfortable in contact lensesabout 5 years ago
ODs look back on 2020about 5 years ago
Long-term follow-up of angiod streaksabout 5 years ago
Can AI rescue physicians from EHR woes?about 5 years ago
How to handle dry eye follow-up visitsabout 5 years ago
Quiz: Know the ocular effects of eyelash growth serumsabout 5 years ago
Know the ocular effects of eyelash growth serumsabout 5 years ago
Quiz answers: Know the ocular effects of eyelash growth serumsabout 5 years ago
How to manage orbital fracturesabout 5 years ago
Navigate postop IOP control with wound burpingNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.