- May digital edition 2021
- Volume 13
- Issue 5
Embrace, don’t fear, AI in diabetic retinopathy
Automated detection of disease helps patients as well as doctors
Challenges exist in diagnosing and grading diabetic retinopathy (DR). Multiple analyses show that many patients with diabetes are not receiving dilated eye examinations at recommended intervals, with increased rates of nonadherence among racial minorities and economically disadvantaged persons.1-3 Eye care providers sometimes incorrectly grade the severity of DR when compared with standardized grading from image reading centers.4-6 Moreover, recent post hoc analysis of data from a major clinical trial involving patients with moderately severe or worse nonproliferative DR (NPDR) being serially followed and treated by retina specialists showed a significant minority of subjects had their DR severity undergraded by those specialists when compared with the image reading center.7
In private conversations with several retinal specialists, they have expressed, in essence, “I don’t know how severe a given patient’s DR is until I see the results of wide-field fluorescein angiography.”
Grading DR severity
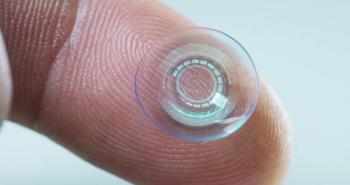
One strategy for addressing these gaps in DR identification and accurate staging is artificial intelligence (AI) retinal imaging algorithms that deploy machine learning to help detect and stage the disease. Two such systems currently have FDA approval for autonomously detecting more than mild DR: IDx-DR (Digital Diagnostics) and EyeArt AI Screening System (EyeNuk, Inc). Both allow nonophthalmic health care personnel to screen patients with diabetes for the presence of DR and assess levels of severity that warrant evaluation by an eye care specialist.
The EyeNuk algorithm allows secondary grading of vision-threatening DR and features a practitioner mode that allows eye care professionals to grade DR severity independently of AI, then compare that grading with the AI grading. Third-party adjudication (EyeScreen Human + AI Diagnostic Service) is available in cases of disagreement.
Clinical studies
Clinical validation results of both algorithms show good detection and accuracy statistics. IDx-DR produced 87.2% sensitivity and 90.7% specificity for more than mild DR (Early Treatment Diabetic Retinopathy Study[ETDRS] level 35 or higher) in a trial of 900 subjects compared with University of Wisconsin’s Fundus Photograph Reading Center assessment.8 EyeArt showed 91.3% sensitivity and 91.1% specificity for more than mild NPDR in 101,710 consecutive patient encounters, and 98.5% sensitivity for referable DR in 6353 patient encounters, defined as more than moderate NPDR (ETDRS level 47 or higher) or diabetic macular edema (DME), when compared with certified image graders in the EyePACS DR telescreening program.9
AI systems potentially help primary care providers ensure that patients with diabetes receive retinal evaluations despite not scheduling or keeping appointments with eye doctors for dilated eye examinations. The systems may also help providers and health systems improve their diabetes care quality metrics (ie, Healthcare Effectiveness Data and Information Set [HEDIS] scores). EyeNuk stratifies DR severity in a way that might drive patients at high risk for diabetes into eye care providers’ offices sooner and potentially augments the providers’ ability to decide which patients require referral to a retinal specialist for consideration of treatment (eg, patients with moderately severe or worse NPDR, proliferative DR, or macular edema).
AI grading
One example of a patient with DR graded by me and the EyeNuk system is seen in Figure 1. This patient had moderate intraretinal hemorrhages and modest vein beading in 2 quadrants of each eye, along with early DME OD that was confirmed by optical coherence tomography (OCT). Submission of macula- and disk-centered 45˚ color retinal images for each eye yielded an AI grading of vision-threatening DR in both eyes in less than 2 minutes from submission, consistent with my clinical diagnosis of severe NPDR OU with DME OD. This patient presented with 20/20 corrected acuities, and the AI grading helped confirm my recommendation for referral to a retina specialist.
Let me be very clear: I am a proponent of inperson eye examinations and expert diagnosis and staging of DR by experienced eye care practitioners in a human environment that facilitates patient engagement regarding prevention, diagnosis, and treatment options. These AI systems are not perfect statistically or from a patient treatment perspective.
For example, I think patients with mild NPDR should see whether they have minimal DR so that they can be educated on steps to prevent progression. AI systems also depend on the acquisition of high-quality images, do not yet evaluate the retinal periphery for DR lesions that portend greater risk of progression, and do not yet employ OCT, the most sensitive tool for detecting and staging DME, the leading cause of vision loss from diabetes.
Conclusion
Patients with diabetes should visit an eye care specialist for annual examinations to detect other diseases or conditions in addition to detecting or staging DR. Eye examinations are also an excellent way to deliver diabetes-specific patient education that reinforces or expands on advice from other providers. The best strategy primary care providers can deploy for improving rates of DR screening is to foster expressly open and collaborative relationships with experienced and technologically savvy eye care providers in their own communities rather than purchase redundant apparatus that serves just one, albeit vital, aspect of managing the care of patients with diabetes. AI represents an opportunity to help prevent blindness in underserved communities with poor access to health care in the United States and worldwide.
It may help eye care practitioners improve their staging and referral acumen and ensure delivery of therapy to patients who are most likely to benefit from it. AI is not a cure-all for DR detection and staging, but it might help to preserve vision at a population level and improve care. AI advancements are unlikely to take anyone’s job, but they will likely make for better doctors.
References
1. Lundeen EA, Wittenborn J, Benoit SR, Saaddine J. Disparities in receipt of eye exams among Medicare part B fee-for-service beneficiaries with diabetes - United States, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(45):1020-1023. doi:10.15585/mmwr.mm6845a3
2. Tran EMT, Bhattacharya J, Pershing S. Self-reported receipt of dilated fundus examinations among patients with diabetes: Medicare expenditure panel survey, 2002-2013. Am J Ophthalmol. 2017;179:18-24. doi:10.1016/j.ajo.2017.04.009
3. Eppley SE, Mansberger SL, Ramanathan S, Lowry EA. Characteristics associated with adherence to annual dilated eye examinations among US patients with diagnosed diabetes. Ophthalmology. 2019;126(11):1492-1499. doi:10.1016/j. ophtha.2019.05.033
4. Scott IU, Bressler NM, Bressler SB, et al; Diabetic Retinopathy Clinical Research Network Study Group. Agreement between clinician and reading center gradings of diabetic retinopathy severity level at baseline in a phase 2 study of intravitreal bevacizumab for diabetic macular edema. Retina. 2008 Jan;28(1):36-40. doi:10.1097/ IAE.0b013e31815e9385
5. Gangaputra S, Lovato JF, Hubbard L, et al. ACCORD Eye Research Group. Comparison of standardized clinical classification with fundus photograph grading for the assessment of diabetic retinopathy and diabetic macular edema severity. Retina. 2013;33(7):1393-1399. doi:10.1097/ IAE.0b013e318286c952
6. Srinivasan S, Shetty S, Natarajan V, Sharma T, Raman R. Development and validation of a diabetic retinopathy referral algorithm based on single-field fundus photography. PLoS One. 2016;11(9):e0163108. doi:10.1371/journal. pone.0163108
7. Kent C. Is it time to treat presymptomatic DR? Review of Ophthalmology. August 10, 2020. Accessed March 20, 2021. https://www.reviewofophthalmology.com/article/is-it-time-totreat- presymptomatic-dr
8. Abràmoff MD, Lavin PT, Birch M, Shah N, Folk JC. Pivotal trial of an autonomous AI-based diagnostic system for detection of diabetic retinopathy in primary care offices. NPJ Digit Med. 2018;1:39. doi:10.1038/s41746-018-0040-6
9. Bhaskaranand M, Ramachandra C, Bhat S, et al. The value of automated diabetic retinopathy screening with the EyeArt system: a study of more than 100,000 consecutive encounters from people with diabetes. Diabetes Technol Ther. 2019;21(11):635-643. doi:10.1089/dia.2019.0164
Articles in this issue
over 4 years ago
What to look for in a telehealth vendorover 4 years ago
Your future telehealth programover 4 years ago
The safest way to fire a staff memberover 4 years ago
ODs can fill need for postconcussion vision rehabover 4 years ago
Tips for preventing ocular zoom fatigueover 4 years ago
Using surveys to help manage dry eye diseaseover 4 years ago
From pipeline to prescription: New drug approval processover 4 years ago
OCT in glaucoma management: Green isn’t always cleanNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.