- August digital edition 2020
- Volume 12
- Issue 8
Peer-reviewed literature answers 3 questions about COVID-19 and conjunctivitis
A look at recent studies informs on incidence, reservoir of virus, and portal of entry
Some 18 million novel coronavirus cases have been reported worldwide. As the eye care community re-opens their practices, important questions about the virus and the eye need to be answered in order to determine the best ways to resume patient care safely and effectively:
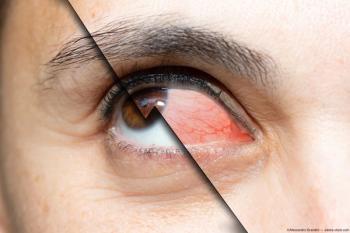
1. What is the incidence of conjunctivitis in patients with COVID-19?
2 . Can the ocular surface serve as a reservoir of virus possibly transmissible to others?
3. Can the ocular surface serve as a portal of entry for COVID-19 through aerosolized droplets or hand-eye contact?
To answer the questions, our research team conducted a comprehensive search of scientific literature databases and analyzed the results of studies in peer-reviewed publications (PubMed) and in scientific preprints (BioRxIV, MedRxIC).
Results of clinical studies
Two large studies reported the incidence of conjunctivitis to be low.1,2 The incidence was 0.8 percent in a study of 1,099 patients with confirmed virus examined by non-eye doctors1 and 4.68 percent in a study of 534 symptomatic confirmed virus cases examined by eye doctors.2
Two case reports described bilateral, acute, follicular conjunctivitis after the onset of respiratory symptoms.3,4 One patient presented 13 days after the onset of symptoms and the other patient, one day after the onset of symptoms. Polymerase chain reaction identified the presence of viral ribonucleic acid (RNA) in conjunctival swabs in both patients.
Another case report described a patient presenting with simultaneous onset of cough, nasal congestion, pre-auricular node ipsilateral to follicular conjunctivitis, and corneal pseudo-dendrites that were initially mistaken for herpetic keratitis. Nasopharyngeal and conjunctival swabs tested positive for Sars-CoV-2.5
Yet another case report, based on a telemedicine consult, presented a patient with unilateral conjunctivitis without systemic symptoms. He did develop fever and headache 3 hours after the ocular consult and tested positive for Sars-CoV-2. No conjunctival swabs were obtained.6
Three additional studies confirmed low incidence of conjunctivitis in patients with confirmed COVID-19. In all 3 studies, viral RNA was identified in most patients with conjunctivitis.
A study of 30 patients with confirmed COVID-19 found that only 1 patient had conjunctivitis.7 Viral RNA was isolated from his conjunctiva. Some 29 patients without conjunctivitis were negative for COVID RNA but had sputum tests positive for the virus.
In a study of 72 patients, 2 patients had conjunctivitis, one of whom tested positive for viral RNA in his conjunctiva.8 Patients without conjunctivitis tested negative for viral RNA in their conjunctivas.
In a study of 63 patients, 1 patient had conjunctivitis and viral RNA has been identified in the conjunctival scrapings.9 In this patient, conjunctivitis was the first presenting sign of COVID-19 with the other, flu-like symptoms quickly following.
A study of tears in 17 patients with a confirmed diagnosis of COVID-19 revealed no viral RNA during the course of their diseases even in one out of 17 patients who developed conjunctivitis.10
In summary, 6 out of 8 patients with conjunctivitis had conjunctival swabs positive for viral RNA. The presence of conjunctivitis should, therefore, be highly suspicious for the presence of COVID-19 virus. The examiner should treat these patients as highly infectious, with very high likelihood that they are shedding virus from their ocular surfaces. On the other hand, patients without conjunctivitis, even if they have other COVID-19 symptoms and should also be treated as highly infectious, are unlikely to harbor viral RNA on their ocular surfaces.
How the virus works
ACE2 receptors are the portals on the surface of human cells by which the virus enters the cells. These receptors are part of the renin-angiotensin system that is instrumental in regulating fluid and electrolyte homeostasis. In addition to their presence in lung, intestine, kidney, blood vessels, heart, and brain tissue, ACE2 receptors have been identified in the trabecular meshwork, ciliary body, and retina, as well as on human corneal epithelial and conjunctival cells.11,12
This, however, raises the question about the low incidence of conjunctivitis compared with respiratory tract infection. One of the reasons could be that the density of ACE2 receptors on the ocular surface is at least 50 percent lower than in other tissues.13 In addition to ACE2, coronaviruses need heparan sulfate co-receptors on the cell surface to facilitate viral binding. Such receptors have been detected on the eye. They are located, however, on corneal dendritic cells and conjunctival fibroblasts, which lie beneath the ocular surface and are not immediately accessible to the virus.14
Lactoferrin and the ocular microbiome
Important proteins in human tears, such as lactoferrin, have been shown to have strong antiviral activity against many viruses. Lactoferrin binds to ACE2 heparan sulfate co-receptors, blocking the virus from attaching to the receptor.15 In several recent studies, liposomal formulation of lactoferrin has been shown to prevent SARS-CoV-2 binding to cells.16
The ocular surface may also be protected by the “good” bacteria and viruses living in thisdistinctive micro-environment, called ocular microbiome, as described in the pioneering article by Anthony St. Leger, PhD.17 In this article, Dr. St. Leger identifies the microbiome on the ocular surface and its effects on the eye’s immune homeostasis and defense against pathogens. In a recent personal communication, Dr. St. Leger shared an observation that the eye’s microbiome may keep the number of ACE2 receptors low and the amount of lactoferrin high to protect the eye against the virus.
Answers to the 3 questions
Returning to the previously mentioned questions, the incidence of conjunctivitis in published studies is low. It is a typical mild-to-moderate viral follicular conjunctivitis with conjunctival injection and watery discharge. Conjunctivitis can be the first presenting sign of COVID-19 or present later in the disease course with a duration of 4 to 7 days.
Regarding the question of the eye as a potential viral reservoir, 6 of 8 patients with conjunctivitis had conjunctival swabs positive for viral RNA. Only 1 of 161 COVID-19 patients without eye symptoms had a positive conjunctival swab, but that patient had other symptoms of viral infection, including fever and cough.
Regarding the question of the ocular surface being a portal of entry for COVID-19 virus, the potential is there but currently has not been proven. While the ocular surface has receptors that virus uses to initiate its attachment to a human cell, other components of the ocular surface may prevent viral attachment and entry.
Recommendations for eyecare providers
Questions about ocular symptoms should be added to the other questions about systemic symptoms asked of patients during screening before they enter the clinic. The ocular questions should include specific references to eye redness, tearing, discomfort, foreign body sensation, and discharge. Clinicians have to decide if their clinic can care for patients with a high probability of shedding the virus or whether they should be triaged to a center fully prepared to safely manage such patients.
If patients have conjunctivitis, clinicians should have high suspicion that they will be shedding virus from their ocular secretions and are, therefore, contagious. In this case, more than hand sanitizer and mask are needed. Clinicians should wear gloves when examining such patients and then immediately discard the gloves using the same precautions as when discarding highly contagious waste material. Clinicians should also assume that symptomatic patients have virus in their nasopharyngeal secretions and that the virus likely will be aerosolized when they speak. Therefore, wearing an N95 mask and tight-fitting goggles is essential. Patients should be instructed to not speak when the examiner is in close proximity to them.
On the other hand, if patients have neither systemic nor ocular signs and/or symptoms suggestive of COVID-19, the probability of them harboring the virus on their ocular surface is very low. When examining such patients, good hand hygiene and face mask are still important for both the patient and the examiner, but goggles and respirator masks may not be necessary. A recent review in Frontiers of Public Health recommends using chlorhexadine/alcoholic hand rub rather than alcohol alone.18
References
1. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Apr 30;382(18):1708-1720.
2. Chen L, Deng C, Chen X, Zhang X, Chen B, Yu H, Qin Y, Xiao K, Zhang H, Sun X. Ocular manifestations and clinical characteristics of 534 cases of COVID-19 in China: a cross-sectional study. MedRxiv. Available at:
3. Chen L, Chen L, Liu M, Zhang Z, Qiao K, Huang T, Chen M, Xin N, Huang Z, Liu L, Zhang G, Wang J. Ocular manifestations of a hospitalized patient with confirmed 2019 coronavirusdisease. Br J Ophthalmol. 2020 Jun;104(6):748-751.
4. Colavita F, Lapa D, Carletti F, Lalle E, Bordi L, Marsella P, Nicastri E, Bevilacqua N, Giancola ML, Corpolongo A, Ippolito G, Capobianchi MR, Castilletti C. SARS-CoV-2 isolation from ocular secretions of a patient with COVID-19 in Italy with prolonged viral RNA detection. Ann Intern Med. 2020 Apr 17;M20-1176.
5. Cheema M, Aghazadeh H, Nazarali S, Ting A, Hodges J, McFarlane A, Kanji JN,Zelyas N, Damji KF, Solarte C. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID-19). Can J Ophthalmol. 2020 Apr 2;55(4):e125-e129.
6. Daruich A, Martin D, Bremond-Cignac D. Ocular manifestations as first sign of Coronavirus Disease 2019 (COVID-19): Interest of telemedicine during the pandemic context. J Fr Ophthalmol. 2020 May;43(5)389-391.
7. Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. Jun;92(6):589-594.
8. Sun X, Zang X, Chen X, Chen L, Deng C, Zou X, Liu W, You H. The infection evidence of SARS-CoV-2 in ocular surface: a single center cross-sectional study. MedRxIV. Available at:
9. Zhou Y, Zeng Y, tong Y, Chen CZ. Ophthalmologic evidence against the interpersonal transmission of 2019 novel coronavirus through conjunctiva. MedRxiv. Available at:
10. Yu Jun IS, Anderson DE, Zheng Kang AE, Wang L, Rao P, Young BE, Lye DC, Agrawal R. Assessing viral shedding and infectivity of tears in Coronavirus Disease 2019 (COVID-19) patients. Ophthalmology. 2020 Jul;127(7):977-979.
11. Napoli PE, Nioi M, d’Aloja E, Fossarello M. The ocular surface and the coronavirus disease 2019: does a dual ocular route exist? J Clin Med. 2020 Apr 28;9(5):1269.
12. Zhou L, Xu Z, Castiglione GM, Soiberman US, Eberhart CG, Duh EJ. ACE2 and TMPRSS2 are expressed on the human ocular surface, suggesting susceptibility to SARS-CoV-2 infection. Ocul Surf. 2020 Jun 13;18(4):537-44.
13. Wilcox MD, Walsh K, Nichols JJ, Morgan PB, Jones LW. The ocular surface, coronaviruses and COVID-19. Clin Exp Optom. 2020 Jul;103(4):418-424.
14. Mayer WJ, Mackert MJ, Kranebitter N, Messmer EM, Grüterich M, Kampik A, Kook D. Distribution of antigen presenting cells in the human cornea: correlation of in vivo confocal microscopy and immunohistochemistry in different pathologic entities. Curr Eye Res. 2012 Nov;37(11):1012-8.
15. Lang J, Yang N, Deng J, Liu K, Yang P, Zhang G, Jiang C. Inhibition of SARS pseudovirus cell entry by lactoferrin binding to heparan sulfate proteoglycans. PLos One. 2011;6(8):e23710
16. Serrano G, Jochergina J, Albors A, Diaz E, Oroval M, Hueso G, Serrano JM. Liposomal lactoferrin as potential preventative and cure for COVID-19. Int J Res Health Sci. 2020;8(1):8-15.
17. St Leger AJ, Desai JV, Drummond RA, Kugadas A, Almaghrabi F, Silver P, Raychaudhuri K, Gadjeva M, Iwakura Y, Lionakis MS, Caspi RR. An Ocular Commensal Protects against Corneal Infection by Driving an Interleukin-17 Response from Mucosal γδ T Cells. Immunity. 2017 Jul 18;47(1):148-158.e5.
18. Sun CB, Wang Y-Y, Liu G-H, Liu Z. Role of the eye in transmitting human coronavirus: what we know and what we do not know. Front Public Health. 2020 Apr 24;8:155.
Articles in this issue
over 5 years ago
3 steps to managing scleral lens patients with allergiesover 5 years ago
3 reasons to fit kids with contact lensesover 5 years ago
Dry eye intranasal spray stimulates the trigeminal nervesover 5 years ago
Technology for optometry post COVID-19over 5 years ago
5 essential truths to treating dry eye diseaseover 5 years ago
How the tear film affects IOL measurementsover 5 years ago
The evolving standard of care in AMDover 5 years ago
Optimizing ocular blood flow in glaucoma managementover 5 years ago
The time is now for optometry and telehealthover 5 years ago
IPL: The science of comfort and safetyNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.