- April digital edition 2021
- Volume 13
- Issue 4
Should ODs get a COVID-19 vaccine and require staff to get vaccinated?
Explore the risks and benefits of different approaches to virus vaccination
With 2020 behind us but hardly forgotten, coronavirus disease 2019 (COVID-19) remains dominant in local, state, and national headlines. New cases of COVID-19 infections and death rates attributed to the virus set records in parts of the United States in the first quarter of 2021.
As the health care system continues to struggle with caseloads and managing this pandemic, the economy seeks to rebound as quickly and safely as possible. Many sectors have taken huge financial losses, yet most optometry practices have survived, albeit with lingering personal protective equipment costs, enhanced cleaning procedures, occasional closures due to COVID-19 cases and/or government edicts, facility and procedural modifications, altered appointment schedules, increased telemedicine usage, and other pandemic-induced adjustments. How close we are to controlling the pandemic and returning to “normal” now seems to hinge on the rollout of COVID-19 vaccines.
Available vaccines
In addition to the final COVID-19 relief package at the end of last year (“What ODs Need to Know About the New COVID Relief Package,” April 2020), 2020 also gave us literal “shots in the arm” on its way out with the FDA’s December 2020 emergency use authorization (EUA) for the first 2 COVID-19 vaccines by Pfizer-BioNTech and Moderna–National Institute of Allergy and Infectious Diseases, respectively. Both represent a novel type of vaccine using messenger RNA to produce immunity and require 2 inoculations separated by several weeks.
Other vaccines showed promising early results by the start of 2021, including those from Oxford-AstraZeneca (a 2-dose vaccine approved and rolled out in the United Kingdom in late 2020 and in India in early 2021) and Johnson & Johnson, both of which use viral vectors to induce immunity. Novavax and others have vaccines in various stages of development, some of which represent traditional protein-based vaccines and require only a single dose.1,2 However, as of the writing of this article, no vaccines to prevent COVID-19 had been FDA approved (ie, none have yet completed the approval process). Instead, we have only these with EUA, indicating the potential benefits outweigh the potential risks.
Vaccination priority
As the first COVID-19 vaccine approvals loomed and subsequent rollouts began in late 2020, the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC) released recommended guidelines for COVID-19 vaccination priority. ACIP’s recommendations were accepted by the CDC and defined “health care personnel” as “paid and unpaid persons serving in health care settings who have the potential for direct or indirect exposure to patients or infectious material.” Guidelines dictate these persons should be prioritized for the COVID-19 vaccine.3
ODs serve in inpatient and outpatient health care settings with the potential for direct and indirect exposure to patients or infectious material, so ODs and their staff members are prioritized in the earliest phase 1a timetable. However, state health agencies are not obligated to follow ACIP’s recommendations, and many—appropriately—prioritized health care workers directly caring for patients with COVID- 19 in hospital settings first, as well as vulnerable residents of long-term care facilities. After these 2 groups, most health care providers in ambulatory and outpatient clinics are next in line.
Do the vaccines work?
Data show how vaccines protect against infection:
– Pfizer’s vaccine is 95% effective at preventing COVID-19.4
– Moderna’s vaccine is 94.1% effective at preventing symptomatic COVID-19.5
– AstraZeneca’s vaccine was found to be 70.4% effective in early studies.6
An individual naturally infected with the virus appears unlikely to become reinfected in the 90 days after initial infection, according to available data,7 but it is too early to know how long the vaccines provide immunity. Vaccines appear to reach maximum efficacy 1 to 2 weeks after the second dose.8
Both vaccines appear to be highly effective at preventing symptomatic COVID-19, but it is too early to conclude whether they reduce transmission of the virus.5 It is anticipated they will be effective against mutations of the virus.8
Adverse events
Although the FDA’s EUA means the potential benefits of these vaccines outweigh their potential risks, adverse events exist. Allergy to any vaccine component is possible, but aside from a rare severe allergic reaction, no concerning safety events were reported, with local reactions (ie, pain, edema, erythema) at the injection site being mild. After the second dose of the vaccine, about half of patients in one study experienced moderate-to-severe adverse events (eg, fatigue, muscle aches, joint pain, headache), which resolved in most patients within 2 days.4,5
Cost
FDA-approved COVID-19 vaccine doses purchased with taxpayer dollars are available to US citizens at no cost; however, health care personnel administering them can charge an administration fee for providing the inoculation. This fee is typically covered by the patient’s public or private medical insurance or, if a patient is uninsured, by the Health Resources and Services Administration’s Provider Relief Fund.7 In some states, ODs are administering vaccinations and are eligible for reimbursement.
Getting vaccinated
Among providers in medical specialties, those in ophthalmology (and by extension, optometry, because ODs provide the same primary eye care, use the same equipment, and are in the same proximity to patients) have been found to be the third most at risk for contracting COVID-19, behind anesthesiology and emergency medicine providers.9 Thus, eye care providers and their staffs are at greater risk of contracting and unwittingly transmitting COVID-19.
Further, the Health Policy Institute of the American Optometric Association provides data indicating a 300% increase in ODs reporting that they or a staff member received a diagnosis or tested positive for COVID-19 during a 3-month period from June to September, 2020.10 These data were collected prior to the most recent record-setting surge in cases.
Vaccines can accelerate “herd” immunity against COVID-19. Although the percentage of the population who needs to be vaccinated to achieve that status is still unclear, certainly the more people who get vaccinated, the faster this immunity will happen.2
Employer-mandated vaccines
The US Equal Employment Opportunity Commis(EEOC) allows employers to mandate vaccinations for employees; however, a mandate can get complicated for disabled employees, those who claim a sincerely held religious practice or belief prohibiting vaccinations, or those with preexisting health conditions for which a vaccine may be contraindicated.
The EEOC states: “If an employee cannot get vaccinated for COVID-19 because of a disability or sincerely held religious belief, practice, or observance, and there is no reasonable accommodation possible, then it would be lawful for the employer to exclude the employee from the workplace. This does not mean the employer may automatically terminate the worker. Employers will need to determine if any other rights apply under the EEO laws or other federal, state, and local authorities.”11
ODs who mandate that staff receive COVID-19 vaccination should develop a written policy and review it with them, recognizing they may need to make “reasonable accommodations” (eg, allowing remote work if the job description permits) unless there is a “significant risk of substantial harm to the health or safety of the individual or others that cannot be eliminated or reduced by reasonable accommodation.”11
Specifically, an employer must individually assess “whether a direct threat exists: the duration of the risk; the nature and severity of the potential harm; the likelihood that the potential harm will occur; and the imminence of the potential harm” before terminating an employee for not receiving a vaccination.11 Consult a labor attorney for additional guidance before making a final decision.
Conclusion
The choice to get vaccinated is personal, at times complicated by institutional distrust, lack of knowledge, misinformation, and fear. To make the best decision possible, ODs should educate staff about these vaccines and their implications for personal and public health, then consider all factors, including relative risk of contracting COVID-19 and possible results if so; the potential health impact on coworkers, patients, friends, and family members; and the safety data and guidance published by the FDA, CDC, and other entities. If desired, practitioners can give staff incentive by allowing them to get vaccinated during working hours and offering to cover out-of-pocket costs.
ODs and their staffs continue to play a crucial role in caring for patients during this unprecedented public health emergency. In so doing, they have a risk of contracting COVID-19 despite mitigation efforts, and vaccines offer an opportunity to help protect one another while accelerating a return to normal.
References
1. Zimmer C, Corum J, Wee SL. Coronavirus vaccine tracker. New York Times. Updated March 16, 2021. Accessed March 16, 2021. https://www. nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html
2. Landscape of novel coronavirus candidate vaccine development worldwide. World Health Organization. March 12, 2021. Accessed March 16, 2021. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines
3. Dooling K, McClung N, Chamberland M, et al. The Advisory Committee on Immunization Practices’ interim recommendation for allocating initial supplies of COVID-19 vaccine—United States, 2020. MMWR. Morb Mortal Wkly Rep. 2020;69:1857-1859. doi:10.15585/mmwr.mm6949e1
4. Pfizer-BioNTech COVID-19 vaccine frequently asked questions. FDA. January 28, 2021. Accessed March 16, 2021. https://www.fda.gov/ emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/pfizer-biontech-covid-19-vaccine-frequently-asked-questions
5. Peer-reviewed report on Moderna COVID-19 vaccine publishes. National Institutes of Health. December 30, 2020. Accessed March 16, 2021. https://www.nih.gov/news-events/news-releases/peer-reviewed-report-moderna-covid-19-vaccine-publishes
6. Knoll MD, Wonodi C. Oxford-AstraZeneca COVID-19 vaccine efficacy. Lancet. 2021;397(10269):72-74. doi:10.1016/S0140- 6736(20)32623-4
7. Frequently asked questions about COVID-19 vaccination. Centers for Disease Control and Prevention. Updated March 12, 2021. Accessed March 16, 2021. https://www.cdc.gov/coronavirus/2019- ncov/vaccines/faq.html
8. Wise N, Moriarty C. The new COVID-19 vaccine: answers to all the hard questions. Yale Medicine. December 18, 2020. Accessed March 16, 2021. https://www.yalemedicine.org/news/covid-19-vaccine
9. Eldred SM. Which specialties are at highest risk for contracting COVID-19? Medscape. May 14, 2020. Accessed March 16, 2021. https://www.medscape.com/viewarticle/930553
10. CDC vaccine prioritization. American Optometric Association. December 3, 2020. Accessed March 16, 2021. https://www.aoa.org/ AOA/Documents/Advocacy/Letters/CDC-Vaccine-Prioritzation.pdf
11. What you should know about COVID-19 and the ADA, the Rehabilitation Act, and other EEO laws. US Equal Employment Opportunity Commission. Updated December 16, 2020. Accessed March 16, 2021. https://www.eeoc.gov/wysk/what-you-should-know-about-covid-19-and-ada-rehabilitation-act-and-other-eeo-laws
Articles in this issue
almost 5 years ago
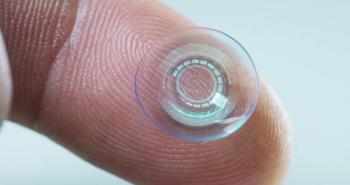
The coming presbyopia revolutionalmost 5 years ago
Biologic medications: The basics that every OD should knowalmost 5 years ago
How to fit scleral lenses with confidence and cautionalmost 5 years ago
Quiz: How to fit scleral lenses with confidence and cautionalmost 5 years ago
Investigational agent aims to eradicate Demodex mitesalmost 5 years ago
Where golf and optometry meetings intersectalmost 5 years ago
News updates April 2021almost 5 years ago
5 glaucoma management mythsalmost 5 years ago
Treating sight-threatening retinopathy using OCTANewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.