- March digital edition 2022
- Volume 14
- Issue 3
5 diabetes truisms that are (at least partially) false
Addressing common misconceptions can help avoid misconstrued scientific facts
Many people, including patients with
Their truth, however, depends on specific factual assumptions, eg, the sun has not vanished forever by cosmological or supernatural means, observers are not wearing a blackout cloak and otherwise have the capacity to detect the sun’s rising, etc.
In philosophy, truisms refer to factual statements that the overwhelming majority of humans believe to be true and do not require fidelity with reality.1 Precisely for this reason, truisms may serve as instruments of both power and deception.
Here, I will attempt to convincingly dispense with at least some of this diabetes flapdoodle.
UNTRUISM #1: Type 2 diabetes (T2DM) is a lifestyle disease attributable to poor patient choices.
We know that excess consumption of highly refined carbohydrates and processed fats contributes to abdominal obesity that drives insulin resistance underlying T2DM.2 However, there are a myriad of other nonlifestyle factors that are causally linked to T2DM, including:
- genetic influences (eg, alteration of mitochondrial DNA in mothers with diabetes that modulates transmission to offspring)3;
- particulate air pollution causing complement system activation, infl ammation, and insulin resistance, leading to T2DM, rates of which are significantly higher in residential proximity to traffic density4,5;
- increased ambient indoor air temperatures (causally linked to T2DM)6;
- communities and workplaces that are engineered to reduce the need for walking/ standing/movement7;
- hypothalamic insulin resistance that drives insatiable hunger despite the stomach being full8,9;
- widespread environmental contamination with obesogenic, endocrine-disrupting contaminants like pesticides, and small-particle plastics that leach into food and water supplies10;
- high prevalence of material inequality and food insecurity in even the wealthiest nations (a predicament 80% more common in diabetes and 240% more common in those with DR)11 that fuels consumption of low-cost, high-sugar/ high-calorie foods with low nutrient density as well as production of stress hormones causally linked to T2DM12;
- increased light exposure prior to sleep—from both indoor LED screen use and outside sources—that negatively affects sleep quality and insulin sensitivity13; and excess antibiotic use reducing intestinal microbiome diversity that modulates insulin sensitivity, thereby increasing diabetes risk.14
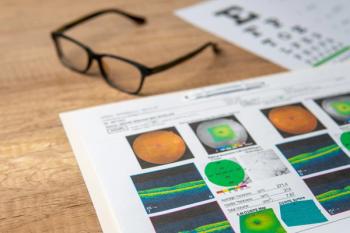
Nearly half of American adults have diabetes or prediabetes.15 It’s time to recognize that the world we have created promotes development of both disorders, irrespective of “personal choice” (see Figure 1).
UNTRUISM #2: Diabetes is like pregnancy—you either have it or you don’t.
This is patent baloney and inconsistent with the gradual pathogenesis of many diseases. There is a long, continuous dysglycemic road on the way to developing diabetes. Insulin response in those with normal blood glucose who subsequently develop T2DM is elevated years before meeting diagnostic thresholds.16
Glucose thresholds for diagnosing diabetes are, in fact, somewhat arbitrary and rates of cardiovascular and microvascular complications (ie, retinopathy) are signifi cantly higher in people with prediabetes having glucose levels that fall below these thresholds.17
Remission of T2DM with bariatric surgery and fasting regimes also vitiates against the view that diabetes is all or nothing. A prominent prediabetes researcher presenting at the European Association for the Study of Diabetes Annual Meeting 2021 recently quipped that “prediabetes, simply, is an early stage of diabetes.”18 Patients can, in fact, have a “touch” of diabetes just like they can have preperimetric glaucoma or high-risk macular drusen with good visual acuity.
UNTRUISM #3: Glycated hemoglobin (HbA1c) measures patients’ average blood glucose levels.
This one is half true. It has been shown that patients with the same HbA1c values may have significantly dissimilar mean blood glucose levels when assessed by validated continuous glucose monitoring systems. For example, a patient with an HBA1c level of 9% may have a better mean glucose than a patient with an HBA1c of 7%.19 High HbA1c is defi nitely a risk factor for development of microvascular complications and is related to mean glucose levels, but it is not the gold standard we once believed it to be.
UNTRUISM #4: A patient’s current HbA1c reflects their risk for DR incidence and progression.
HbA1c is merely a snapshot—a less-than-perfect one, given No. 3 above—of glycemic status over a 60- to 90-day period. Multiple randomized clinical trials have shown that long-term glycemic control, especially in the fi rst 10 years, has more impact on the development of DR than current control.20
This phenomenon, called metabolic memory (see “
Ideally, patients will also have access to their glucose time-in-range (TIR; percentage of time glucose values range between 70 and 180 mg/dl) and time-above-range (TAR) via CGMS, values that predict diabetic retinopathy independently of HbA1c.21
UNTRUISM #5: Eye doctors should base decisions to refer and treat vision threatening DR (severe NPDR, PDR and DME) on patients’ current HbA1c because patients with excellent control are unlikely to progress or experience vision loss.
Posthoc analysis of the PANORAMA trial (NCT02718326), which randomized patients with moderately severe or severe nonproliferative diabetic retinopathy (NPDR) without diabetic macular edema (DME) to either observation (usual care) or injections of aflibercept for 100 weeks, showed that patients with “good” glycemic control at study entrance were slightly more likely to progress to proliferative disease or DME than were patients with worse glucose control.22
Multiple patients who progressed to NPDR/ DME in this trial had HbA1c levels < 6.5% at study entrance. The same lack of protection was also found with respect to diabetes duration and body mass index (ie, neither low/ high BMI nor shorter/longer duration of diabetes protected against development of PDR/ DME in this cohort. This may be a reflection of long-term glucose levels (metabolic memory), the inadequacies of A1c, and/or other factors that have yet to be determined. This means that any patient with more than moderate NPDR should be considered for anti-VEGF therapy. The horse is already out of the barn.
These are a few of the most important fallacies that pervade our diabetes consciousness. Others include the following:
- Clinical examination by retina specialists accurately stages DR severity in all cases.
- Only obese patients develop T2DM.
- All patients with long-term diabetes will ultimately develop sight-threatening DR.Patients who experience diabetes-related vision loss have only themselves to blame.
- Dilated retinal exams are no longer important with the use of ultrawide-fi eld retinal imaging.
- ODs are in no position to critically evaluate the overall diabetes treatment plan.
All of these, like what precedes them, are partial or total nonsense, baloney, balderdash, malarkey, moonshine, and flapdoodle. Don’t be duped. Tell a friend.
References
1. Oxford English Dictionary. Truisms. Accessed January 19, 2022. https:// www.oed.com/
2. McEvoy CT, Cardwell CR, Woodside JV, Young IS, Hunter SJ, McKinley
MC. A posteriori dietary patterns are related to risk of type 2 diabetes: findings from a systematic review and meta-analysis. J Acad Nutr Diet. 2014;114(11):1759-75.e4. doi:10.1016/j.jand.2014.05.001
3. Zheng, LD, Linarelli LE, Liu L, et al. Insulin resistance is associated with epigenetic and genetic regulation of mitochondrial DNA in obese humans. Clin Epigenetics. 2015;7(1)60. doi:10.1186/s13148-015-0093-1
4. Yang M, Cheng H, Shen C, et al. Effects of long-term exposure to air pollution on the incidence of type 2 diabetes mellitus: a meta-analysis of cohort studies. Environ Sci Pollut Res Int. 2020;27(1):798-811. doi:10.1007/ s11356-019-06824-1
5. Zhao Z, Lin F, Wang B, Cao Y, Hou X, Wang Y. Residential proximity to major roadways and risk of type 2 diabetes mellitus: a meta-analysis. Int J Environ Res Public Health. 2016;14(1):3. doi:10.3390/ijerph14010003
6. Speakman J, Heidari-Bakavoli S. Type 2 diabetes, but not obesity, prevalence is positively associated with ambient temperature. Sci Rep. 2016;6:30409. doi:10.1038/srep30409
7. Hamilton MT, Hamilton DG, Zderic TW. Sedentary behavior as a mediator of type 2 diabetes. Med Sport Sci. 2014;60:11-26. doi:10.1159/000357332
8. Kullmann S, Valenta V, Wagner R, et al. Brain insulin sensitivity is linked to adiposity and body fat distribution. Nat Commun. 2020;11(1):1841. doi: 10.1038/s41467-020-15686-y
9. Isganaitis E, Lustig RH. Fast food, central nervous system insulin resistance, and obesity. Arterioscler Thromb Vasc Biol. 2005;25(12):2451- 2462. doi:10.1161/01.ATV.0000186208.06964.91
10. Kumar M, Sarma DK, Shubham S, et al. Environmental endocrinedisrupting chemical exposure: role in non-communicable diseases. Front Public Health. 2020;8:553850. doi:10.3389/fpubh.2020.553850
11. Kirby JB, Bernard D, Liang L. The prevalence of food insecurity is highest among Americans for whom diet Is most critical to health. Diabetes Care. 2021;44(6):e131-e132. doi:10.2337/dc20-3116
12. Berm dez-Mill n A, Wagner JA, Feinn RS, et al. Inflammation and stress biomarkers mediate the association between household food insecurity and insulin resistance among Latinos with type 2 diabetes. J Nutr. 2019;149(6):982-988. doi:10.1093/jn/nxz021
13. Nagai N, Ayaki M, Yanagawa T, et al. Suppression of blue light at night ameliorates metabolic abnormalities by controlling circadian rhythms. Invest Ophthalmol Vis Sci. 2019;60(12):3786-3793. doi:10.1167/iovs.19- 27195
14. Yuan J, Hu YJ, Zheng J, et al. Long-term use of antibiotics and risk of type 2 diabetes in women: a prospective cohort study. Int J Epidemiol. 202049(5):1572-1581. doi:10.1093/ije/dyaa122
15. US Centers for Disease Control and Prevention. National Diabetes Statistics Report 2020. Reviewed August 28, 2020. Accessed January 19, 2022. www.cdc.gov/diabetes/data/statistics-report/index.html
16. Sagesaka H, Sato Y, Someya Y, et al. Type 2 diabetes: when does it start? J Endocr Soc. 2018;2(5):476-484. doi:10.1210/js.2018-00071
17. Baranowska-Jurkun A, Matuszewski W, Bandurska-Stankiewicz E. Chronic microvascular complications in prediabetic states-an overview. J Clin Med. 2020 Oct;9(10):3289. doi:10.3390/jcm9103289
18. Sehauser C. Prediabetes: Does It Really Matter? Paper presented at the EASD Prediabetes Symposium; September 30, 2021.
19. Beck RW, Connor CG, Mullen DM, Wesley DM, Bergenstal RM. The fallacy of average: how using HbA1c alone to assess glycemic control can be misleading. Diabetes Care. 2017;40(8):994-999. doi: 10.2337/dc17- 0636
20. Zhang L, Chen B, Tang L. Metabolic memory: mechanisms and implications for diabetic retinopathy. Diabetes Res Clin Pract. 2012;96(3):286-293. doi:10.1016/j.diabres.2011.12.006
21. Gabbay MAL, Rodacki M, Calliari LE, et al. Time in range: a new parameter to evaluate blood glucose control in patients with diabetes. Diabetol Metab Syndr. 2020;12:22. doi:10.1186/s13098-020-00529-z
22. Brown DM, Wykoff CC, Boyer D, et al. Evaluation of intravitreal aflibercept for the treatment of severe nonproliferative diabetic retinopathy: results from the PANORAMA randomized clinical trial. JAMA Ophthalmol. 2021;139(9):946-955. doi:10.1001/ jamaophthalmol.2021.2809
Articles in this issue
almost 4 years ago
Keeping calm with positive vibesalmost 4 years ago
Addressing the need for greater access in vision carealmost 4 years ago
Tackling the problem of contact lens dropout from presbyopiaalmost 4 years ago
The ideal glaucoma patient, from an optometrist’s perspectivealmost 4 years ago
5 reasons optometrists have failed to embrace myopia managementalmost 4 years ago
Contoured prism lenses enhance vision clarity and patient comfortalmost 4 years ago
Restoring sight against all oddsNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.