- January digital edition 2021
- Volume 13
- Issue 1
5 things to get your patients ready for cataract surgery
Educate patients preoperatievly, evaluate their needs, and set appropriate expectations
Every day, I see patients who have been referred for cataract surgery—but have unfortunately been sent to us without any of the preparation that will ensure a smooth and satisfactory experience for the patient, and a painless postoperative management experience for the referring optometrist.
Here are 5 things I wish every doctor discussed with their patients before referring them for surgery.
1. Discuss the existence of lifestyle lenses
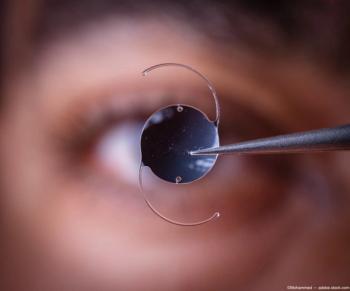
A surgical practice has to provide true informed consent, so we will certainly talk to every patient who is a candidate about presbyopia- and astigmatism-correcting intraocular lens (IOL) options. But the reality is that this topic is best introduced early on, while the patient has the time and energy to think about what is important for their lifestyle and budget.
The preoperative consultation is a long one. The patient will see several different doctors, counselors, and technicians; go through a lot of diagnostic testing; and will likely be tired and somewhat overwhelmed by the end of the visit.
That’s a terrible time to introduce a major decision for the first time. That doesn’t mean that we want everyone to get a lifestyle lens. But we don’t want them to throw up their hands and say “Oh, just give me the standard!” and then later regret a decision made in haste.
2. Truly evaluate the patient’s needs
A primary eyecare provider who has an established relationship with the patient knows so much more about that patient than the surgeon can learn in a short appointment.
Consider and share all the elements that are relevant to the IOL choice and refractive targets, including:
– The state of the accommodative system
– History of astigmatism and presbyopia correction in glasses or contact lenses
– Most important distances for the patient’s daily activities
– Frequency of night driving
– How easily satisfied the patient is with his spectacle or contact lens prescription
– Unusual avocations that require specialized lenses or have non-negotiable distance requirements
For example, as an instrument-rated private pilot I have to be able to see the instrument panel clearly (Figure 1). If my IOL doesn’t allow for that, I will need glasses for the cockpit.
This isn’t about telling the patient, “Hey, I want you to have XYZ lens.” Ultimately, the surgeon will determine which lens type and lens power to implant, but she needs information to make the best choice.
3. Carefully explain range of vision
When talking to patients about how important near vision is for them, it is important to be very, very clear because this is easily misunderstood. “Near” is a very subjective term.
I like to hand patients a near card upside down. The need to turn it around will force them to naturally reposition the card where they like to hold reading material. Depending on patients’ height and arm length, where they typically position devices, and what their hobbies are, “near” can mean anything from embroidery at 6 inches to a computer screen at 36 inches.
A simple way to explain the concept to patients is this: “If you have a standard lens implanted, you won’t be able to see anything clearly that you can touch. There are lens options (such as Tecnis Symfony [Johnson & Johnson Vision]) that can provide a natural range of high-quality vision that will satisfy most patients.”
Someone with short arms or a fine-detail hobby may need a lens that is designed for a closer near-point (such as PanOptix [Alcon] or Tecnis Multifocal IOLs).
It is really important to physically demonstrate to low myopes what their vision will be like with a standard IOL. These patients will almost certainly discount whatever you say about this if you don’t show them. Low myopes have breezed through presbyopia just by removing their glasses to see up close. They believe they will retain this natural ability!
So, ODs need to put lenses with their full correction in front of their eyes and ask them to look at a near target, explaining that it will always be this way once they have cataract surgery. With a demonstration like this, I have found that many low myopes would much rather have a presbyopia-correcting lens that offers the range of vision they expect to have.
Similarly, if the patient has always had astigmatism correction in his glasses and is excited to be able to see at distance after cataract surgery, he needs to understand that no matter how good the surgeon is, he will still need glasses unless he opts for astigmatism correction at the time of surgery.
4. Evaluate and treat ocular surface disorders
Patients with dry eye—whether symptomatic or not—must be treated before preoperative measurements are taken, to ensure that the biometry and IOL power selection are accurate. If they come in for a consult with undiagnosed and untreated dry eye, that slows down the process tremendously because the surgical practice must postpone measurements and start treatment.
The first question a patient always asks is, “Why didn’t Dr. Smith tell me I had this?”
It is an awkward situation for the surgical practice to manage, and it generally causes the patient to lose confidence in the referring doctor. Moreover, it means the referring doctor has ignored the practice opportunity to offer billable treatment services.
5. Set appropriate expectations
Every IOL offers advantages and disadvantages, including standard monofocal IOLs. A prepared patient understands what she is getting into, regardless of the direction she chooses.
Patients who choose a presbyopia-correcting IOL, and especially if they might get a multifocal IOL, need to understand the potential for night vision symptoms. You can explain that the starbursts they currently see at night (because of the cataract) won’t entirely go away, but they will be less noticeable.
I like to explain neuroadaptation to patients by demonstrating physiological diplopia. Tell the patient to hold a finger about 12 inches from his face. Then hold a pencil at arms’ length. Tell the patient, “When you look at your finger, you are still aware of the pencil, right?” While looking at his finger but being aware of the pencil, he will now see 2 pencils.
I explain, “Your brain naturally adapts to this phenomenon so you don’t go around seeing double when focused at a specific distance, but if you concentrate, you can see it. Night vision symptoms are a lot like that. The blurred image is there, but your brain will tune it out.”
And of course, if the patient chooses a standard monofocal IOL, he needs to know to expect that he will need glasses for some or all tasks, as discussed in the third point.
The most important factor in maintaining your patients’ trust after surgery—and having a smooth and trouble-free postoperative course—is taking the time to educate patients preoperatively so they are not unpleasantly surprised by the results.
Articles in this issue
almost 5 years ago
Imaging to differentiate disc drusen from papilledemaalmost 5 years ago
Gonioscopy and imaging work in tandemalmost 5 years ago
Contact lens trends during COVID-19almost 5 years ago
Blepharitis requires patient educationalmost 5 years ago
How to implement IPL into an optometry practicealmost 5 years ago
How ODs can address patients lost to follow upalmost 5 years ago
What ODs need to know about the new COVID-19 relief packageabout 5 years ago
ODs look to what 2021 will bringNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.