- January digital edition 2021
- Volume 13
- Issue 1
How ODs can address patients lost to follow up
Practitioners need to educate and stress the importance of additional care
Lost to follow-up (LTFU) is a widespread phenomenon encompassing all aspects of health care. Though the term applies strictly to clinical trials, it is broadly used in reference to routine and specialty care delivered by healthcare professionals to patients in clinical practice who do not return for successive monitoring and/or treatment after a new care or treatment regimen has begun.1 LTFU in clinical care is sometimes referred to as “follow-up non-attendance” (FUNA).
Factors in LTFU
In regards to systemic management of
• Younger age
• Lower socioeconomic and education status
• Lower diabetes knowledge
• Male gender
• Both lower and higher HbA1c
• Longer disease duration
• Insulin use
• Multiple diabetes comorbidities
• Smoking
• Less frequent eye examination intervals
The same analysis cited multiple patient reasons for FUNA, particularly beliefs that specific patients’ diabetes was not that serious or had remitted, lack of access to transportation and affordability of care, and workplace commitments.3
LTFU/FUNA is typically classified as complete (patient is never again seen by the original provider) or partial (follow-up occurs, but less often than is required by clinical trial protocol or recommended by real-world healthcare providers).2
LTFU in eye care
Given this multiplicity of factors, it is not surprising that LTFU/FUNA is commonplace in eye care as well. From a surveillance standpoint, studies show that 21 percent to 53 percent of patients with diabetes fail to adhere to recommended intervals for dilated eye examinations.4,5 Of course, the majority of patients do not have sight-threatening diabetic eye disease at any given time, so the impact of less-than-optimal examination frequency for detection of diabetic retinopathy (DR) and diabetic macular edema (DME) is mitigated if and when patients ultimately do return for eye examination (partial LTFU/FUNA), though disease severity may be worse and the potential for consequential vision loss is substantially higher.
What is more surprising, perhaps, is the high number of patients who are diagnosed with sight-threatening diabetic eye disease yet do not follow through with a complete course of therapy from treating ophthalmologists.
Retrospective analysis of 2595 DME patients over 5 years found that about 25 percent of patients who received at least 1 anti-VEGF injection did not return for subsequent injections within the next 12 months, with higher rates of LTFU among Asian and Latino Americans, and those with annual income < $50,000.6
For proliferative diabetic retinopathy (PDR), studies show that 25 to 52 percent are LTFU/FUNA at 12 months.7,8 Odds of LTFU increased in Black, Hispanic, Native and Pacific Island Americans, those with income <$40,000, non-native English speakers, and those <55 years of age.
In 1 study of outcomes in PDR patients LTFU for at least 6 months, patients receiving anti-VEGF therapy in isolation versus pan-retinal photocoagulation in isolation were more than 10 times as likely to have developed traction retinal detachment upon subsequent follow-up, though the numbers of eyes were small and final visual acuity was not significantly different.9
Another questionnaire analysis of 76 patients LTFU with PDR showed a significant positive correlation between best-corrected visual activity (BCVA) loss and patient’s lack of trust and satisfaction with treatment.10
Optometrists must recognize that many patients with diabetes do not receive eye examinations at appropriate intervals, do not necessarily follow through with referrals to retinal specialists (only 51 percent of patients with vision-threatening DR were seen by a retinal specialist within 12 months of referral in one recent analysis of 407 patients11), and do not complete treatment regimens for sight-threatening eye disease.
This underscores the need for ODs to stress the importance of not only receiving dilated retinal examinations but keeping referral appointments and ongoing treatment by retina specialists.
Of note, poor follow-up among patients with DR, glaucoma, and/or AMD was also highly associated with poor patient knowledge of their diagnoses.12 Subjects partially or totally LTFU identified the following strategies to improve follow-up: contact with others having the same eye condition (41.3 percent), greater education regarding eye disease (40.8 percent), and improved transportation services to the clinic (44.6 percent).
Along with other epidemiological factors discussed above, ODs must be particularly cognizant of those patients at higher risk and redouble their efforts to preserve vision through disease-specific patient education, timely referral and follow-up, and collaborative communication among eyecare providers and other members of the diabetes care team, including patients and their advocates.
Case example
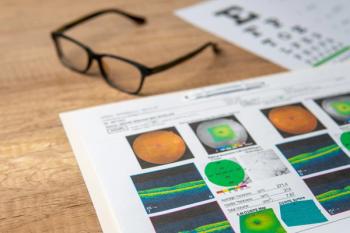
This is a 32-year-old male with type 1 diabetes for 21 years. His metabolic control had been poor (HbA1c ranging from 8 to 12 percent since diagnosis) and presented with fibrovascular proliferation, vitreous hemorrhage, and severe vision loss in 2013 due to PDR (Figure 1). He underwent vitrectomy with endolaser PRP and returned with much improved retinal status and 20/60 visual acuity in 2014 (Figure 2). At that time, HbA1c had improved to 7.6 percent and glucose time-in-range over 90 days was 72 percent by continuous glucose monitoring system (Medtronic Guardian RT).
In 2015, he was found to have recurrent neovascularization of the optic nerve by the treating retinal specialist. He received a single injection of bevacizumab (Avastin, Genentech) and was instructed to return in 4 weeks for further anti-vascular endothelial growth factor (VEGF) treatment. He was LTFU and returned to my office 14 months later with a traction retinal detachment and 20/800 vision in that eye (Figure 3).
This case underscores the importance of early, good metabolic control in mitigating the risk of sight-threatening diabetic retinopathy (so-called “protective metabolic memory”) as well as the critical importance of preventing LTFU in patients with severe disease.
References
1. Grimsrud AT, Cornell M, Egger M, Boulle A, Myer L. Impact of definitions of loss to follow-up (LTFU) in antiretroviral therapy program evaluation: variation in the definition can have an appreciable impact on estimated proportions of LTFU. J Clin Epidemiol. 2013 Sep;66(9):1006-1013.
2. Malcolm JC, Maranger J, Taljaard M, Shah B, Tailor C, Liddy C, Keely E, Ooi T. Into the abyss: diabetes process of care indicators and outcomes of defaulters from a Canadian tertiary care multidisciplinary diabetes clinic. BMC Health Serv Res. 2013 Aug 10;13:303.
3. Griffin SJ. Lost to follow-up: the problem of defaulters from diabetes clinics. Diabet Med. 1998 Nov;15 Suppl 3:S14-24.
4. Fisher MD, Rajput Y, Gu T, Singer JR, Marshall AR, Ryu S, Barron J, MacLean C. Evaluating adherence to dilated eye examination recommendations among patients with diabetes, combined with patient and provider perspectives. Am Health Drug Benefits. 2016 Oct;9(7):385-393.
5. Eppley SE, Mansberger SL, Ramanathan S, Lowry EA. Characteristics associated with adherence to annual dilated eye examinations among US patients with diagnosed diabetes. Ophthalmology. 2019 Nov;126(11):1492-1499.
6. Gao X, Obeid A, Aderman CM, Talcott KE, Ali FS, Adam MK, Rovner BW, Hyman L, Ho AC, Hsu J. Loss to follow-up after intravitreal anti-vascular endothelial growth factor injections in patients with diabetic macular edema. Ophthalmol Retina. 2019 Mar;3(3):230-236.
7. Obeid A, Gao X, Ali FS, Talcott KE, Aderman CM, Hyman L, Ho AC, Hsu J. Loss to follow-up in patients with proliferative diabetic retinopathy after panretinal photocoagulation or intravitreal anti-VEGF injections. Ophthalmology. 2018 Sep;125(9):1386-1392
8. Suresh R, Yu HJ, Thoveson A, Swisher J, Apolinario M, Zhou B, Shal AR, Fish RH, Wykoff CC. Loss to follow-up among patients with proliferative diabetic retinopathy in clinical practice. Am J Ophthalmol. 2020 Jul;215:66-71.
9. Obeid A, Su D, Patel SN, Uhr JH, Borkar D, Gao X Fineman MS, Regillo CD, Maguire JI, Garg SJ, Hsu J. Outcomes of Eyes Lost to Follow-up with Proliferative Diabetic Retinopathy That Received Panretinal Photocoagulation versus Intravitreal Anti-Vascular Endothelial Growth Factor. Ophthalmology. 2019 Mar;126(3):407-413.
10. Abdelmotaal H, Ibrahim W, Sharaf M, Abdelazeem K. Causes and clinical impact of loss to follow-up in patients with proliferative diabetic retinopathy. J Ophthalmol. 2020 Feb 8;2020:7691724.
11. Bresnick G, Cuadros JA, Khan M, Fleischmann S, Wolff G, Limon A, Chang J, Jiang L, Cuadros P, ER Pederson. Adherence to ophthalmology referral, treatment and follow-up after diabetic retinopathy screening in the primary care setting. BMJ Open Diabetes Res Care. 2020 Jun;8(1):e001154.
12. Thompson AC, Thompson MO, Young DL, Lin RC, Sanislo SR, Moshfeghi DM, Singh K. Barriers to follow-up and strategies to improve adherence to appointments for care of chronic eye diseases. Invest Ophthalmol Vis Sci. 2015 Jul;56(8):4324-31.
Articles in this issue
almost 5 years ago
Imaging to differentiate disc drusen from papilledemaalmost 5 years ago
Gonioscopy and imaging work in tandemalmost 5 years ago
5 things to get your patients ready for cataract surgeryalmost 5 years ago
Contact lens trends during COVID-19about 5 years ago
Blepharitis requires patient educationabout 5 years ago
How to implement IPL into an optometry practiceabout 5 years ago
What ODs need to know about the new COVID-19 relief packageabout 5 years ago
ODs look to what 2021 will bringNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.