- November digital edition 2020
- Volume 12
- Issue 11
How diabetes affects COVID-19
Considerations for eyecare providers to better care for their patients with diabetes
As of this writing, the global
Diabetes and COVID-19
Although patients with diabetes are not believed to be more susceptible to primary infection by the virus, the presence of diabetes is now a well-established risk factor for poor outcomes, including higher risk of intensive care unit (ICU) admission, ventilatory intubation, and death. After obesity and hypertension (conditions that frequently commingle with diabetes),
The reasons for this increased risk are not entirely clear, but diabetes in general, and hyperglycemia and insulin resistance in particular, are linked to excess inflammation, vascular coagulability, and increased risk of secondary infection, including pneumonia.6 Diabetic ketoacidosis (DKA) is occurring at higher rates in patients with diabetes and
Recent analysis of
Specifically, patients with a spot blood glucose reading >196 mg/dl (11.1 mmol/L) at admission were 3.2 times more likely to experience in-hospital complications (including more than a doubled risk of ARDS and ICU admission, and nearly a 10-fold increased risk of acute cardiac injury) and 7.6 times more likely to die compared to patients with blood glucoses <196 mg/dL.10
Further analysis has also shown that patients with diabetes with relatively good metabolic control prior to admission (with a predominance of glucose readings between 70 and 180 mg/Dl and/or glycosylated hemoglobin <7.5 percent) had better outcomes than those with poorer relative glucose control.11 Moreover, fasting blood glucose >126 mg/ dl compared with <106 mg/dl in admitted patients without previous diagnosis of diabetes increased mortality 4-fold over the next month in 605 hospitalized COVID-19 patients in Wuhan, China.12
In addition to promoting inflammation and clotting, analysis shows that glycosylation (irreversible glucose binding) of angiotensin conversion enzyme type-2 (ACE2) receptors is requisite for spike protein attachment of SARS-CoV-2 to epithelial cells, a feature that may explain why hyperglycemia is such a profound risk factor for poor outcomes.13 In concert with clinical outcomes data discussed above, this had led many diabetologists to advocate for far more rigorous control of hyperglycemia when
Additionally, many suggest discontinuation of sodium glucose cotransporter type-2 reuptake inhibitors (SGLT2i), a newer class of diabetes medicine that facilitates urinary excretion of glucose and has demonstrated cardioprotective and renoprotective benefit in large clinical trials but also increases the risk of DKA and may increase ACE2 receptor activity.15 Interestingly, a clinical trial is now specifically looking at the potential heart and kidney benefits of SGLT2 therapy in patients with newly-diagnosed SARS2-CoV infection.16
Increased mortality
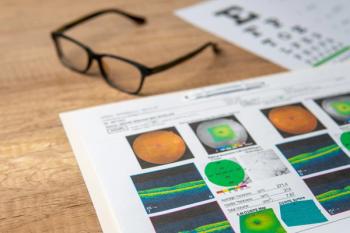
All this begs the question as to whether or not patients with diabetes should be examined by optometrists and ophthalmologists at customary intervals for the presence and worsening of diabetic retinopathy.
As Socrates is purported to have said: It depends. Although diabetes patients do not appear to be more likely to contract COVID-19 infection when outside the home than are other patients, the reality is that patients with diabetes are significantly more likely to suffer complications and die, particularly if their metabolic control is poor.
In all cases, increased susceptibility to morbidity and mortality from COVID-19 infection in
Delaying eye exams
Although patients with sub-optimal control are also at higher risk for developing diabetic retinopathy in general and sight-threatening diabetic retinopathy in particular, it may be prudent to delay routine dilated eye examinations for at least some of these patients (such as those with no or relatively mild non-proliferative diabetic retinopathy and no evidence of macular edema the year before) to minimize risk of community exposure in-transit to and within busy eyecare facilities.
For patients with no retinopathy and good glucose control, the decision to delay makes even more sense. For patients with sight-threatening retinopathy (severe non-proliferative diabetic retinopathy [NPDR], proliferative diabetic retinopathy [PDR] and/or diabetic macular edema [DME]) the need for close follow-up and treatment, if indicated, to preserve vision almost certainly outweighs the risk.
The UK Center for Evidence Based Medicine (CEBM) has expeditiously generated recommendations for diabetic retinopathy exam intervals during this pandemic calling for surveillance intervals of 18 to 24 months in low-risk patients and customary follow-up intervals for those who require laser photocoagulation or anti–vascular endothelial growth factor (anti-VEGF) therapy.17 CEBM also advocates for in-office infection control measures as outlined above.
We live in extraordinary times that have required ODs to adapt to the “new normal” for safe delivery of eye care. Staying up-to-date on community-specific transmission of COVID-19, giving sound advice, and tailoring clinical protocols for patients at high-risk will allow ODs to preserve patients’ vision, well-being, and lives.
References
1. Worldometer. COVID-19 Coronavirus Pandemic. Available at: https://www.worldometers.info/coronavirus/. Accessed 8/19/20
2. Vincent JL, Taccone FS. Understanding pathways to death in patients with COVID-19. Lancet Respir Med. 2020 May 1;8(5):430-432.
3. Li X, Ma X. Acute respiratory failure in COVID-19: is it “typical” ARDS? Crit Care. 2020 May 6;24(1):198.
4. Dhont S, Derom E, Van Braeckel, EV, Depuydt P, Lambrecht BN. The pathophysiology of ‘happy’ hypoxemia in COVID-19. Respir Res. 2020 Jul 28;21(1):198.
5. Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidsom KW, the Northwell COVID-19 Research Consortium; Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J, Coppa K, Diefenbach MA, Dominello AJ, DuerHefele J, Falzon L, Gitlin J, Hajizadeh N, Harvin TG, Hirschwerk DA, Kim EJ, Kozel ZM, Marrast LM, Mogavero JN, Osorio GA, Qiu M, Zanos TP. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020 May 26;323(20):2052– 2059.
6. Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020;8(9):782-792.
7. Palermo NE, Sadhu AR, McDonnell ME. Diabetic Ketoacidosis in COVID-19: Unique Concerns and Considerations. J Clin Endocrinol Metab. 2020 Aug 1;105(8):dgaa360.
8. Goldman N, Fink D, Cai J, Lee YN, Davies Z. High prevalence of COVID-19-associated diabetic ketoacidosis in UK secondary care. Diabetes Res Clin Pract. 2020 Aug;166:108291.
9. Korytkowski M, Antinori-Lent K, Drincic A, Hirsch IB, McDonnell ME, Rushakoff R, Ranganath Muniyappa R. A Pragmatic Approach to Inpatient Diabetes Management during the COVID-19 Pandemic. J Clin Endocrinol Metab. 2020;105(9):dgaa342.
10. Li Y, Han X, Alwalid O, Cui Y, Cao Y, Liu J, Gu J, Wang L, Fan Y, Shi H. Baseline characteristics and risk factors for short-term outcomes in 132 COVID-19 patients with diabetes in Wuhan China: A retrospective study. Diabetes Res Clin Pract. 2020 Aug;166:108299.
11. Zhu L, She ZG, Cheng X, Qin JJ, Zhang XJ, Cai J, Lei F, Wang H, Xie J, Wang W, Li H, Zhang P, Song X, Chen X, Xiang M, Zhang C, Bai L, Xiang D, Chen MM, Liu Y, Yan Y, Liu M, Mao W, Zou J, Liu L, Chen G, Luo P, Xiao B, Zhang C, Zhang Z, Lu Z, Wang J, Lu H, Xia X, Wang D, Liao X, Peng G, Ye P, Yang J, Yuan Y, Huang X, Guo J, Zhang BH, Li H. Association of Blood Glucose Control and Outcomes in Patients with COVID-19 and Pre-existing Type 2 Diabetes. Cell Metab. 2020 Jun 2;31(6):1068-1077.e3.
12. Wang S, Ma P, Zhang S, Song S, Wang Z, Ma Y, Xu J, Wu F, Duan L, Yin Z, Luo H, Xiong N, Xu M, Zeng T, Jin Y. Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: a multi-centre retrospective study. Diabetologia. 2020 Oct;63(10):2102-2111.
13. Zhao P, Praissman JL, Grant OC, Cai Y, Xiao T, Rosenbalm KE, Aoki K, Kellman BP, Bridger R, Barouch DH, Brindley MA, Lewis NE, Tiemeyer M, Chen B, Woods RJ, Wells L. Virus-Receptor Interactions of Glycosylated SARS-CoV-2 Spike and Human ACE2 Receptor. Preprint. bioRxiv. 2020 Jul 24;2020.06.25.172403.
14. Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020 Apr 7;323(13):1239-1242.
15. Chatterjee S. SGLT-2 inhibitors for COVID-19–A miracle waiting to happen or just another beat around the bush? Prim Care Diabetes. 2020 Oct;14(5):564-565.
16. ClinicalTrials.gov. Dapagliflozin in Respiratory Failure in Patients With COVID-19 (DARE-19). Available at: https:// clinicaltrials.gov/ct2/show/NCT04350593. Accessed 8/19/2020.
17. Hunter J, Arentz S, Goldenberg J, Yang G, Beardsley J, Lee MS, Myers SP. Choose your shortcuts wisely: COVID-19 rapid reviews of traditional, complementary and integrative medicine. Integr Med Res. 2020 Sep;9(3):100484.
Articles in this issue
about 5 years ago
Quiz: Treatments for presbyopia coming soonabout 5 years ago
Quiz Answers: Treatments for presbyopia coming soonabout 5 years ago
When to lease and when to own office spaceabout 5 years ago
Vision rehabilitation of patients with strokeabout 5 years ago
Treatments for presbyopia coming soonabout 5 years ago
Novel uses of technology for systemic diseaseabout 5 years ago
Know the pros and cons of outsourcing billingabout 5 years ago
5 communication strategies for dry eye patientsNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.