Optimize diabetes health management
Episodes in this series

Rishi Singh, MD: We’re going to discuss the successful partnership between our optometrists and our medical doctors in taking care of patients with diabetes. Let’s start off with our first question….What education can the optometrist provide a patient with diabetes to help optimize their health?
Steven G. Ferrucci, OD, FAAO: Talking about the asymptomatic nature of diabetic retinopathy and diabetic macular edema until they progress is an important thing. We need to get patients to understand that good vision on an eye chart or in the real world doesn’t necessarily mean that their eyes are healthy. The other thing that is important to educate patients about is metabolic memory, which is the idea that higher blood glucose controlled early has a protective effect 20, 30 years down the line, according to various studies. There was an interesting trial that looked at patients in 36 countries, and it said that these are all patients with Type 2 diabetes, and only about 18% of people 5 years after diagnosis had a glycated hemoglobin [A1C] under 7%, which is ideal, and less than half had a glycated hemoglobin under 8%. We need to harp early on, when diabetes is diagnosed, about the importance of good metabolic control.
The other thing I would stress may be outside of the purview of eye doctors, but I talk about it on a daily basis: if a patient has preexisting cardiovascular disease, we have diabetes medications now that dramatically lower their risk of having a fatal event, such as an MI [myocardial infarction] or a stroke. For patients who have known heart disease, it’s a good idea to talk to them about talking with their PCP [primary care physician] or endocrinologist about these new medications. I’m referring to the GLP-1 [glucagon-like peptide 1] analogues such as Victoza, [liraglutide], Byetta, [exenatide], and the SGLT2 [sodium-glucose cotransporter 2] inhibitors, which are the drugs that end in –flozin, such as Jardiance [empagliflozin] or Farxiga [dapagliflozin].
Rishi Singh, MD: Dr Ferrucci, I have the same question for you. Talk more about this idea of metabolic control. It’s a wide field, right? It could be blood sugar or blood pressure. What do we mean by metabolic control that’s ideal?
Steven G. Ferrucci, OD, FAAO: A lot of studies show us that with better blood sugar control you’re less likely to get diabetic retinopathy. Hopefully, if you have diabetic retinopathy, then you are less likely to have it progress if you have good hemoglobin control. Most places use hemoglobin A1Cas a measure of blood glucose levels. In a perfect world, we want our patients with diabetes at 7% or less. There is some new research going on about different types of parameters that we can use, but I’ve found that it’s helpful to ask our patients if they know what their hemoglobin A1C is because it has been shown in many studies to be a risk factor for development of diabetic retinopathy.
Rishi Singh, MD: We have patients who come into our clinics with various levels of diabetic retinopathy and diabetic macular edema, for that matter. Dr Ferrucci, at what point should an optometrist feel comfortable referring a patient with diabetic retinopathy or diabetic macular edema?
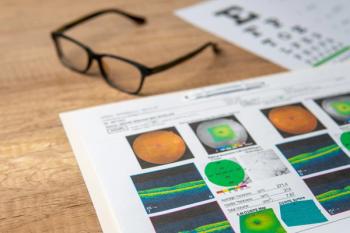
Steven G. Ferrucci, OD, FAAO: That’s an excellent question. First and foremost, it all depends on your own personal situation. I tend to see a lot of patients with diabetes in my practice, so I’m comfortable with patients with diabetes. We all have different levels of comfort, and there’s never a wrong time to get a second opinion if you’re not comfortable. If you look at the American Optometric Association Guidelines that were put out fairly recently, they seem to recommend that we refer over to retinal specialists at the earliest signs of severe nonproliferative diabetic retinopathy, proliferative diabetic retinopathy, and diabetic macular edema, especially center-involved diabetic macular edema. It makes sense when you start to see those types of patients. Those are patients who could benefit from a referral to a retinal specialist to discuss whether some treatment options are a good option at that time.
Rishi Singh, MD: Dr Loewenstein, I’ll get an international perspective from you. When do you want to see patients from other providers who have diabetic macular edema or diabetic retinopathy? Is it the beginning mild retinopathy or is it much more severe?
Anat Loewenstein, MD: No, in Israel, the situation is really different. An optometrist would usually refer a patient for diabetic retinopathy screening if the patient doesn’t have 20/20 vision and if they see something going on in the fundus examination. The patient will be referred early in the course of their disease. I’m comfortable because I work with optometrists all the time. I get a lot of referrals, and I am referring to optometrists, as well, sometimes because of the visual acuity. I’m not as big an expert as the optometrists are on maximal visual acuity. It’s also important sometimes to know what level of visual acuity we have with the patients for the treatment decisions. Even though most of the treatment decisions are based on OCT [optical coherence tomography] imaging, visual acuity may also be an answer to that. I usually get the referral early in the course of the disease in the health system in Israel.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.