Diabetes management challenges
Episodes in this series

Rishi Singh, MD: What we just discussed sounds easy enough, but Dr Ferrucci or Dr Chous, do you want to talk about the common challenges that providers face when treating patients with this condition?
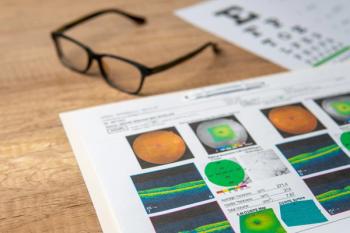
Steven G. Ferrucci, OD, FAAO: Yes, there are obviously a lot of challenges. One of the biggest challenges we sometimes have is something Paul alluded to earlier, which is asymptomatic disease. A lot of people seem to think, “If I see well, then my eyes must be healthy.” I’m sure that we have all seen patients with significant diabetic retinopathy who have perfect 20/20 or near 20/20 vision. It’s an important message to convey to our patients that even if they have good vision, they still need to get their eyes checked on a routine basis. I explain to them that, if there is a problem, I want to know about it as soon as possible because we then have more options for treatment vs waiting too late and then our hands are somewhat tied.
Rishi Singh, MD: Dr Chous, would you like to comment on that?
A. Paul Chous, MA, OD, FAAO: Patients have a lot of physician visits when they have diabetes. On average, it is something like 15 per year, so patients get overwhelmed. We need to stress the importance of eye care, but a lot of patients face financial, food insecurity, and transportation barriers. There is also a phenomena associated with retinopathy called diabetic encephalopathy where cognitive function declines, especially in patients over the long term. Chronic hyperglycemia not only damages the retina, it damages the brain. This is something for which it is often helpful in my practice to have family members in with the patient when I’m discussing when the patient needs to be seen again or why they need to be referred to a retina specialist.
Rishi Singh, MD: Dr Loewenstein, we’ll finish with you on this topic of patients who don’t come back. How do you ensure that they’ll come back to you? Are there mechanisms you’ve found or are there best practices you could share with us about how to have a patient not be lost to follow-up and return to us for treatment?
Anat Loewenstein, MD: Unfortunately, both in my private clinic and in the division that I’m leading in the public hospital, we don’t have a system for that. The only thing is that, in Israel, there is a very good system with primary care physicians such that they’re being quality controlled by the percentage of patients they refer to ophthalmologists. This solved a lot of these follow-up issues because it is the primary care physicians who make sure that the patients are seeing us. For them, it’s a good parameter by which we measure the quality of their work.
Rishi Singh, MD: That’s great. Thank you for that discussion.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.