Using OCT-A for patients with diabetes
Episodes in this series

Rishi Singh, MD: Steve, we talked a little bit about OCT-A [optical coherence tomography angiography] imaging, so I want you to describe it for people who may not be familiar with OCT-A. How does it work? It’s non–dye-based in comparison with the fluorescein angiography we discussed before. Tell us and the watchers at home what it is and why it may be beneficial.
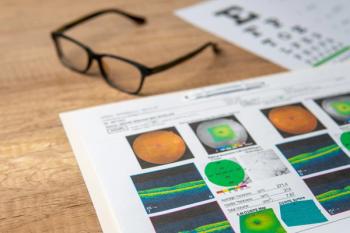
Steven G. Ferrucci, OD, FAAO: The way that OCT-A imaging works, in a simplified way, is this: OCT-A imaging can scan so quickly with so many scans per second that it can scan over a blood vessel and tell whether there’s any flow in that blood vessel over a certain period of time. By doing that, it can extrapolate whether that’s a patent blood vessel that has blood flowing through it or if it’s a blood vessel that doesn’t have any blood, which would be an ischemic blood vessel. It can use that technology without dye to figure out blood flow, blood patterns, and that sort of thing.
Rishi Singh, MD: Tell me about the clinical situations in which OCT-A has been useful to you.
Steven G. Ferrucci, OD, FAAO: I agree that, for all of our diabetic patients, it would be a nice idea to do it, but we don’t. The times I find it helpful is when you have a patient with diabetes who has unexplained vision loss. Their vision is poorer than you think it should be, but they don’t seem to have edema. We’ve used OCT [optical coherence tomography] imaging, and we’ll find some macular ischemia in those patients. It does a good job of looking for macular ischemia in those types of patients.
Rishi Singh, MD: Another area that I’ve found is sometimes a red herring is when you see a patient who is diabetic and has pretty much no retinopathy but they have some temporal microaneurysms in the eye. You may realize that they have JXT [juxtafoveal telangiectasia] or some other masquerade syndrome that might look like it, so I find that OCT-A imaging is helpful in those kinds of cases.
Anat Loewenstein, MD: That’s correct. I agree. If something is not clear, then I would go to OCT-A imaging.
Rishi Singh, MD: Yes, but why hasn’t OCT-A imaging become the standard of care? Should it become the standard of care? This may be for everyone on the panel, so I’ll start with Paul. Should OCT-A imaging be the standard of care? What are the barriers from OCT-A adoption at this point?
A. Paul Chous, OD, MA, FAAO: Cost is certainly a barrier to any technology that’s introduced into the marketplace. The argument has been made that you can pick up on DR [diabetic retinopathy] lesions much earlier with OCT-A imaging than you can with traditional examination techniques. You can see microaneurysms that wouldn’t be visible otherwise.
My question is this: does that really change the treatment the patient is going to receive? It certainly gives you an opportunity to counsel that patient about better metabolic control, and we’re going to watch that patient a bit more closely. There are some patients for whom I’ve used OCT-A imaging where I’ve discovered something I didn’t see on clinical examination, and it freaks them out a bit. They get more concerned than they may have been otherwise, so I have to reassure them that these are early changes. The reality is that adaptive optics shows patients have diabetic retinopathy within 6 months of diagnosis, but the question is this: what does that portend for the future?
Anat Loewenstein, MD: First of all, OCT-A imaging takes longer…than structural OCT. Then I think the interpretation is not that useful. It also takes time to interpret that imaging. It’s not like a structural OCT that the clinician is doing without getting instructions and getting results. If the segmentation is not done in the proper way in OCT-A imaging, then you will not get what you are looking for. For example, if we are talking about patients with diabetes, and 1 of the uses of OCT-A is for patients with diabetes, if you want to see if what is on the retina is MGE [medical ganglionic eminence progenitor cell] or not, you can do the slabs on the anterior surface of the retina, and then you will see them. If you are not doing the slabs in the right place, then you will not see it. This is something that not everyone is aware of, and you are sometimes just doing an OCT-A imaging test, but you are not getting what you are looking for because you didn’t look in the right place. It’s a bit of a barrier. Then, of course, there is also cost as well as the time that it takes to perform the imaging and interpret it. These are all barriers.
Steven G. Ferrucci, OD, FAAO: I would also add that, even though some of the newer ones allow us to see [farther] out, we’re still not getting to the periphery. There are still some limits there that make fluorescein, especially widefield fluorescein, very valuable still.
Rishi Singh, MD: You’re right: OCT-A imaging has limitations in the line scans thus far compared with widefield angiography, so you still can’t get out as far. One of the other things that I can tell you about OCT-A imaging is that reviewing the images is not easy, as Dr Loewenstein pointed out. I find that I spend a lot more time reviewing the images and looking at the slabs. I like the idea of following neovascularization, and I do follow neovascularization on the disc with the OCT-A to see response. We can be fooled into thinking that there is a response to therapy when there truly is not, so it gives you a bit more of a quantitative look at that neovascularization in a patient you might have with that.
Anat Loewenstein, MD: It has a lot of potential in this regard in diabetes especially now that we are talking about treating patients with PDR [proliferative diabetic retinopathy] with anti-VEGF therapy as compared with PRP [panretinal photocoagulation]. You do need to make sure that you don’t have active blood vessels as opposed to PRP, for which you do the PRP and that was practically it. We are now sometimes giving injections, and we are following up with the patients. I personally don’t trust myself to see all these MGEs. I’m not saying that I also have time to do OCT-A imaging all over the retina and make sure that there is no MGE anywhere, but maybe in the future, using the AI [artificial intelligence] or machine learning, we will have a score for that, and it can potentially be helpful in this regard in the future.
Rishi Singh, MD: I want to talk to Dr Loewenstein about the concept of home OCT imaging. What are the pros and cons? How is this technology going to be helpful to screen or assist in diabetes care?
Anat Loewenstein, MD: Theoretically, home OCT imaging can be beneficial. We use the home OCT imaging in patients with diabetes even though most of our studies [at Tel Aviv University] are on patients with AMD [age-related macular degeneration]. All of our longitudinal studies that follow the patients at home over a month’s time were with patients with AMD, but it’s OCT imaging, so you can see the thickness. We also worked on it with our artificial intelligence interpretation system, the NOA [Notal OCT Analyzer] that shows where the intraretinal fluid is and where the subretinal fluid is to know the response to treatment. We don’t have as many studies about the home OCT imaging for patients with diabetes as we do for patients with AMD. Theoretically, it can be beneficial for that, as well. The pace of things that happen in diabetic retinopathy does not necessitate daily OCT imaging, and the main advantage of home OCT imaging is to have the daily examination. It’s more for patients with AMD, but it does have potential for patients with diabetes.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.