- Vol. 11 No. 3
- Volume 11
- Issue 3
New diabetes agents can improve, save patients’ lives
Several diabetes medications are now available for reducing blood glucose levels, with more on the horizon. Such drugs work by a variety of pharmacologic mechanisms. Clinical practice guidelines generally call for using the most effective agents with the greatest historical safety profiles at the lowest cost.
Reducing elevated blood glucose levels has a significant impact on the incidence and severity of
Even more importantly, which medicines patients are prescribed can have a profound impact on the risk of them suffering major adverse cardiovascular events (MACE)- myocardial infarction (MI), cerebrovascular accident (CVA), death from MI or CVA, coronary artery bypass grafting (CABG), or hospitalization for congestive heart failure (CHF).
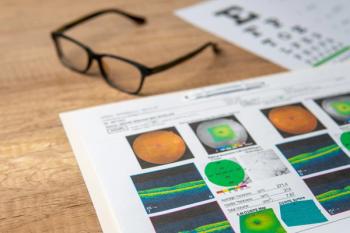
Our goal as eyecare providers is to reduce the risk of significant vision loss caused by diabetes. But we must also keep an eye on preventing MACE. After all, with prevention and treatment options available, most patients will not go blind from diabetes.
However, most patients will suffer cardiovascular disease, which remains the largest cause of mortality in patients who have diabetes.3 Put more plainly, mortality trumps good vision.
Effective medications
Analysis of these cardiovascular outcomes has shined new light on what is meant by using the most “effective” diabetes medications.
This has been gauged primarily by a drug’s potency for absolute reductions in glycosylated hemoglobin (HbA1c) as well as patient tolerance of side effects and drug costs (what agent gives us the biggest and safest “bang for the buck”).
Metformin has long been considered the drug of choice in type 2 diabetes management because it is inexpensive, relatively effective at lowering mean blood glucose, and its use appeared to decrease bad cardiovascular outcomes when compared to patients on either insulin or sulfonylurea medicines in clinical trials.4
Both glucagon-like peptide receptor-1 analogs (GLP-1 RA)-liragutide (Victoza, Novo Nordisk), semaglutide (Ozempic, Novo Nordisk), exenatide (Bydureon, AstraZeneca) and dulaglutide (Trulicity, Eli Lilly)-and sodium-glucose co-transporter type 2 (SGLT2) inhibitors-canagliflozin (Invokana, Eli Lilly) dapagliflozin (Farxiga, AstraZeneca), and empagliflozin (Jardiance, Boehringer Ingelheim)- have been shown to significantly reduce MACE when compared to “usual care” with metformin plus add-on therapy as needed.5,6
Relative risk reductions for various CVD outcomes have been 10 to 15 percent for the GLP-1 agents and 40 to 50 percent for the SGLT2 drugs.
SGLT2 drugs appear to reduce the risk of hospitalization for CHF about 40 percent and preserve/improve kidney function in patients with and without early diabetic kidney disease.7
Cost barriers
Unfortunately, these new drugs’ high prices have limited their use by prescribing physicians.
But because macrovascular complications of diabetes are far costlier to the U.S. economy than microvascular complications, the case for early use of these more expensive agents may gain strength.
The average cost of a coronary artery CABG was roughly $151,000 in 2016,8 a figure that potentially dwarfs the $3,500 to $4,000 annual cost of these newer drugs for high-risk patients.
Patient analysis
Interestingly, the Comparative Effectiveness of Cardiovascular Outcomes in New Users of SGLT-2 Inhibitors (CVD-REAL) study showed that even patients with no prior history of CVA events had an almost 50 percent reduction in heart failure and death with use of any SGLT2 inhibitor.9
Evidence from a 2018 analysis also suggests that sulfonylurea agents as a class may be associated with a greater risk of CV events and mortality,10 including as add-on therapy to metformin.
More than 140,000 U.S. veterans over 14 years of follow-up experienced nearly a 40 percent increase in mortality with sulfonylureas (SFU) compared to add-on pioglitazone (Actos, Takeda).11
The most striking association comes from a meta-analysis comparing patients on GLP-1 analogs or SGLT2 inhibitors to patients using primarily second-generation SFU drugs like glipizide (Glucotrol, Pfizer) or glyburide (Diabeta, Sanofi).
Patients in the latter group had more than a 40-fold increased risk of cardiovascular death or heart attack in the analysis of more than 1.5 million patients (82 randomized trials and 26 observational studies followed for a mean of six years).12
Guidelines in practice
These findings have prompted me to routinely recommend that patients on SFUs-especially glyburide or glipizide-ask their diabetes physicians about substituting GLP-1 (injectable) or SGLT2 (oral) therapy for the SFU, particularly if they have known atherosclerotic disease (either class of agent) or CHF (SGLT2 drugs).
In fact, a 2018 consensus guideline from the American Diabetes Association and the European Association for the Study of Diabetes (EASD) recommends an SGLT2 inhibitor as second-line therapy for type 2 diabetes after metformin (especially in patients with established CV disease).13
Pending release of blood glucose and cardiovascular outcomes data, the Food and Drug Administration’s (FDA) approval of dapagliflozin is also expected for type 1 diabetes within the next year.
The bottom line is that all healthcare providers seeing patients with diabetes should be aware of the potential heart- and life-saving benefits of these new agents.
Frank discussion should be recommended between diabetes patients and their primary care physicians, internists, endocrinologists and/or cardiologists. Tell a friend.
References:
1. Diabetes Control and Complications Trial Writing Group. The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes. 1995 Aug;44(8):968-83.
2. Zhang X, Zhao J, Zhao T, Liu H. Effects of intensive glycemic control in ocular complications in patients with type 2 diabetes: a meta-analysis of randomized clinical trials. Endocrine. 2015 May;49(1):78-89.
3. Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol. 2018;17(1):83.
4. UK Prospective Diabetes Study Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998 Sep 12;352:854-865.
5. Bethel MA, Patel RA, Merrill P, Lokhnygina Y, Buse JB, Mentz RJ, Pagidipati NJ, Chan JC, Gustavson SM, Iqbal N, Maggioni AP, Ohman P, Poulter NR, Ramachandran A, Zinman B, Hernandez AF, Holman RR, EXSCEL Study Group. Cardiovascular outcomes with glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes: a meta-analysis. Lancet Diabetes Endocrinol. 2018 Feb;6(2):105-113.
6. Clegg L, Heerspink HL, Penland RC, Weifeng T, Boulton DW, Bachina S, Fox RD, Fenici P, Thuresson M, Mentz RJ, Hernandez AF, Bethel MA, Holman RR. 130-LB-Impact of SGLT2 inhibitors (SGLT2i) on cardiovascular (CV) risk and estimated glomerular filtration rate (eGFR) in the EXSCEL placebo group. Presented at American Diabetes Association scientific meeting, July 17, 2018, Orlando, FL.
7. Seidu S, Kunutsor SK, Cos X, Gillani S, Khunti K, For and on behalf of Primary Care Diabetes Europe. SGLT2 inhibitors and renal outcomes in type 2 diabetes with or without renal impairment: A systematic review and meta-analysis. Prim Care Diabetes. 2018 Jun;12(3):265-283.
8. Giacomino BD, Cram P, Vaughan-Sarrazin M, Zhou Y, Giortra S. Association of hospital prices for coronary artery bypass grafting with hospital quality and reimbursement. Am J Cardiol. 2016;117(7):1101-1106.
9. Cavender MA, Norhammar A, Birkeland KI, Jørgensen ME, Wilding JP, Khunti K, Fu AZ, Bodegard J, Blak BT, Wittbrodt E, Thuresson M, Fenici P, Hammar N, Kosiborod M, CVD-REAL Investigators and Study Group. SGLT-2 Inhibitors and Cardiovascular Risk: An Analysis of CVD-REAL. J Am Coll Cardiol. 2018 Jun 5;71(22):2497-2506.
10. Powell WR, Christiansen CL, Miller DR. Meta-analysis of sulfonylurea therapy on long-term risk of mortality and cardiovascular events compared to other oral glucose-lowering treatments. Diabetes Ther. 2018 Aug;9(4):1431-1440.
11. Powell WR, Christiansen CL, Miller DR. Long-term comparative safety analysis of the risks associated with adding or switching to a sulfonylurea as second-line type 2 diabetes mellitus treatment in a U.S. veteran population. Diabet Med. 2018 Oct 21. doi: 10.1111/dme.13839.
12. Bain S, Druyts E, Balijepalli C, Baxter CA, Currie CJ, Das R, Donnelly R, Khunti K, Langerman H, Leigh P, Siliman G, Thorlund K, Toor K, Vora J, Mills EJ. Cardiovascular events and all-cause mortality associated with sulphonylureas compared with other antihyperglycaemic drugs: A Bayesian meta-analysis of survival data. Diabetes Obes Metab. 2017 Mar;19(3):329-335.
13. Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, Rossing P, Tsapas A, Wexler DJ, Buse JB. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018 Dec;41(12):2669-2701.
Articles in this issue
almost 7 years ago
Amniotic membrane grafts help ocular surface diseasealmost 7 years ago
Blue light: Why it mattersalmost 7 years ago
Troubleshoot contact lens discomfort and prevent complicationsalmost 7 years ago
Keep an eye on link between glaucoma and blood pressurealmost 7 years ago
Use technology advancements to modernize your practicealmost 7 years ago
Educate, don’t sell to patientsalmost 7 years ago
Know how to care for pediatric patients diagnosed with Down syndromealmost 7 years ago
Legislative session offers opportunity to join inNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.