- February digital edition 2021
- Volume 13
- Issue 2
Review Duane’s retraction syndrome diagnosis and treatment
Understand the condition’s structural, innervational, neurological, and genetic abnormalities
A rare, but well-known restrictive strabismus entity, Duane’s retraction syndrome (DRS), is a type of congenital cranial disinnervation disorder (CCDD).1 The hallmark finding of this non-progressive congenital strabismus is limited horizontal eye movement accompanied by globe retraction, which results in narrowing of the palpebral fissure. It is characterized by cocontraction of horizontal recti on attempted adduction, causing globe retraction along with variable amounts of upshoots or downshoots.1,2
Globe retraction in patients with severe ocular motility limitation was first described by Heuck.3 Others have provided detailed descriptions of DRS.4-8 The description summarizing the findings made by previous studies was published by Alexander Duane in 1905.1 However, in European literature, the syndrome is referred, perhaps more appropriately, as Stilling-Turk-Duane retraction syndrome.
Electrophysiological tests, neuro-imaging, and chromosomal analysis give a better insight into DRS, along with other CCDD disorders. Management strategies for DRS are no longer limited to surgical interventions but optometric vision therapies (OVT) as well.9
Prevalence and epidemiology
DRS accounts for 1% to 5% of strabismus and is found in only about 0.1% of the general population.10,11 DRS is unilateral in 85% of the cases. It is more commonly unilateral than bilateral, affecting the left eye (59%) more often.10-13 The right to left shunt causes embolic phenomena that affect the left carotid artery, causing dysregulated apoptosis followed by misinnervation and ocular malformations.
Interestingly, DRS also has female preponderance.13,15 It is postulated that the more susceptible to the expression of genes responsible for the manifestation of DRS are partly sex-limited with incomplete penetrance in females.13,16 Also, during embryogenesis, higher estrogen levels, along with the greater risk of inflammation, predispose females to venous thromboembolic events.14 Bilateral cases of DRS have been reported to range from 10% to 24% of all DRS cases and are usually associated with asymmetrical involvement.10,17,18
Etiopathogenesis and risk factors
DRS is a spectrum of structural, innervational, neurologic, and genetic abnormalities that influence each other, giving rise to patterns of clinical presentations. A number of risk factors have also been associated with DRS. Some schools of thought are described below.
STRUCTURAL ANOMALIES
Previously, many researchers believed that the globe retraction phenomenon was caused by structural anomalies. Heuck believed that globe retraction on attempted adduction was due to posterior insertion of the medial rectus muscle, causing the faulty medial rectus insertion to act as “retractor bulbi.”3 This view was supported by many other researchers as well.6,19,20
Turk believed that fixation of the globe by non-elastic lateral rectus muscle was the cause of globe retraction on adduction.5
Wolff similarly described a congenitally anomalous lateral rectus, which was inelastic and tight as the cause of abnormal motility in DRS.8
Abnormal vertical eye movements during adduction were also thought to be caused by structural anomalies in which the compensatory oblique overaction replaces the defective abductive action of the lateral rectus muscle.21
Another view is that due to the weak medial rectus muscle, the vertical rectus muscles overact to act as adductors.7 Some researchers have also postulated the phenomenon based on cocontraction of the horizontal recti muscles.22,23
INNERVATIONAL ANOMALIES
Electromyographic studies hint at the possibility of innervation faults to be the cause of retraction more than anatomical anomalies. Breinin studied the electric potentials generated by muscles in various positions of gaze in DRS and found that there was no lateral rectus activity recordable in attempted abduction, while maximum lateral rectus action potentials were generated in adduction, suggesting that the lateral rectus was receiving innervation in adduction.24 This was thought to be the cause of the cocontraction and globe retraction.
Abnormal synergistic innervation between the medial rectus and vertical rectus or oblique muscle was also demonstrated electromyographically, which may explain the vertical deviation in adduction.25 The narrowing of the interpalpebral fissure on adduction is owed to the adjustment of the lids to the retracting globe.
NEUROLOGICAL ABNORMALITIES
The neurological basis of DRS is autopsy based. Recent electrophysiological studies show that the absence of normal innervation to the lateral rectus muscle by the sixth nerve can cause DRS. This can be nuclear in origin or supranuclear (brainstem abnormalities).
Currently, the most favored theory in DRS is due to brainstem abnormalities. The possibility of acquired retraction following brainstem injury gives credence to this thought pattern. Some investigators have found abducens nucleus hypoplasia or complete absence in the brain stem to be the cause of DRS.26,27 Others have proposed that infranuclear abnormalities at the level of cavernous sinus, where the oculomotor and abducens nerves are in the vicinity of each other, leads to features of DRS.28 Evidences such as synkinesis, crocodile tears, and optokinetic-nystagmus further support the neurological basis of DRS.29,30
GENETICS
Familial occurrences of DRS with autosomal inheritance occurs in 10% of cases.1,31 Genetic analysis of the autosomal dominant variant has is associated with mutations in the CHN1 gene, which is known to affect the abducens and less commonly, the oculomotor nerves.
In isolated DRS without systemic association, the DURS1 locus on chromosome 2q31 has been identified and mapped,32,33 while in DRS with associated malformation syndromes, the Duane Radial Ray syndrome has been found to have a dominant inheritance with incomplete penetrance with deletion mutations in SALL4 gene on chromosome.34,35
DRS has been also described in monozygotic twins in which “mirror-image” patterns was observed in unilateral cases.36
EMBRYOPATHIES
DRS is rarely an isolated finding—most commonly, an ocular or systemic association is prevalent. In sporadic cases, Cross and Pfaffenbach proposed an intriguing theory that a common teratogenic stimulus occurs at 8 weeks of gestation, which could be of etiologic significance.37
Fetal alcohol syndrome is associated with DRS in which the developing abducens nucleus is damaged during the first trimester.38 DRS may also be caused by vascular hypofunction during fourth to fifth weeks of embryogenesis as seen in vertebral basilar arterial junction aneurysm.39
DRS also frequently occurs in patients afflicted with thalidomide syndrome.40 These findings suggested that there could be a critical period during embryogenesis, in which an insult could result in various congenital malformations including DRS.40
Besides congenital forms, retraction syndrome can be acquired, which has been referred to as acquired retraction syndrome or Pseudo Duane’s retraction syndrome. Some causes of the acquired form of retraction are shown in Table 1.21,41-49
Classification
Many classification systems have been proposed by different authors, some based on clinical presentation and others on mechanism. Some of the classification system on DRS are shown in Table 2.16,50-54
Huber’s classification system is the most accepted system. It is based on electromyographic results, categorizing DRS into three classes: Type I, II, and III. The order of frequency follows Type I (78%), Type III (15%), and Type II (7%).55,56 Some researchers have attempted to modify Huber’s classification system into subgroups depending upon eye alignment on primary gaze for surgical relevance.
Clinical features and diagnosis
The clinical features of DRS are described in the following subheadings.
REFRACTIVE ERROR
In DRS, hyperopia and hyperopic astigmatism were found to be more common in comparison to myopia, simple myopic astigmatism, and emmetropia.51,57,58 Cases with high hyperopia may also have an accommodative component.
Amblyopia: Anisometropic and ametropic amblyopia have been reported to be the most common causes of amblyopia in DRS, especially unilateral Type I.57-59 Some investigators also reported strabismic amblyopia to be more common.60
Strabismus: In the primary position, esotropia is commonly seen, followed by orthotropia and exotropia. While patients with unilateral Type I have esotropia more frequently than exotropia, those with Type II have exotropia, and those with Type III have esotropia, exotropia, and orthotropia occurring equally.61 Deviation in bilateral DRS is found to be variable.
Motor evaluation of strabismus:
– Ocular motility: The abduction deficit in DRS accompanies a disproportionately smaller primary position deviation. This helps to distinguish it from a sixth nerve palsy where the primary deviation and the abduction limitation are in proportion to each other62
– Nature of deviation: Due to limited motility in lateral gazes, the deviation may vary in vertical and lateral gazes. Bilateral DRS may be more likely to have pattern strabismus, compared to unilateral cases.63 V-pattern strabismus may be commonly seen in DRS. Because A-pattern is more common in bilateral DRS, a thorough evaluation of A-pattern must be performed to inspect DRS. Upshoot and downshoot may give an impression of X-pattern
– Abnormal vertical deviations: While adducting, variable degree of upshoots and downshoots may be observed (Leash Phenomenon). Grading for overshoots64 is shown in Table 3. With the involved eye in adducted position, a straight line parallel to the intermedial canthal line is drawn from the pupillary center of the fellow eye. Upshoots and downshoots may either be mechanical or innervational in origin
– Globe retraction: On attempted adduction, globe retraction occurs due to cocontraction of the extraocular muscle acting as retractor bulbi. With the involved eye in the maximum adducted position, a scale is used at the center of the palpebral fissure width to measure the palpebral aperture height and compared with that of the fellow eye in abduction. Grading for globe retraction64 is shown in Table 4
– Narrowing of palpebral fissure: The palpebral fissures narrows on attempted adduction to adjust for retracting globe. Pseudoptosis and lower lid elevation have also been shown by some investigators
– Abnormal head posture: Head turn is usually adopted by the patient to maintain binocular single vision and to compensate for duction deficits. It is more pronounced in unilateral cases with head turn in the direction of most affected duction
Sensory evaluation of strabismus:
– Diplopia and confusion is rarely a complaint as the patients maintains fusion by abnormal head posture
– Suppression is a rare finding, if found so, abnormal retinal correspondence is present.
– Good stereopsis is seen in most cases.
Phenotypes of DRS: Two variants of DRS have been reported.
Vertical retraction syndrome: In vertical retraction syndrome, instead of limitation on adduction or abduction, variable amounts of limitation of elevation or depression with globe retraction and palpebral fissure narrowing is seen. The affected eye may be orthotropic, hypertropic, or hypotropic in the primary position and may coexist with horizontal retraction. This vertical retraction may be due to innervational anomalies, fibrosis of vertical rectus muscles, or a “tethering” effect of the horizontal rectus.65
Congenital adduction deficit with synergistic divergence: This is a rare phenotype of DRS presenting with unilateral adduction deficit and simultaneous abduction of the eye on attempted adduction.66 On attempted adducting, an abducting nystagmus is seen. It is associated with a head turn to unaffected side with large angle exotropia.
DRS rarely occurs as an isolated finding; it has both systemic and ocular association along with syndromic findings as seen in Table 5.37,67-71
DIFFERENTIAL DIAGNOSIS
Disorders that are similar in presentation to DRS can be acquired as a result of trauma or following localized infection of the orbit leading to inflammation and consequent mechanical restrictions of eye movement.
Acquired DRS can easily be diagnosed based on the history, but congenital isolated DRS is difficult, owing to lack of cooperation among infants. Moreover, retraction, elevation, and depression of the globe on adduction may not be detected until early childhood. Differential diagnosis of DRS are listed in Table 6.
MANAGEMENT
Though DRS has been extensively studied, no standard procedure to restore the normal ocular excursions has been established. The most accepted treatment options for DRS include monitoring, prism, and, in certain cases, surgery.9,55,56,72,73
The management approach for DRS has been focused primarily on surgical methods in presence of abnormal head posture and significant deviation in primary position, although the results are often disappointing; therefore, no clinical trials support the use of surgery for DRS.55,56 Several reports in the literature suggest optometric vision therapy (OVT) as a management option for these patients.9,72
Optical correction: Because refractive error and amblyopia frequently occur in DRS, proper optical correction for any degree of ametropia is crucial management step. In DRS, hyperopia is more prevalent, which may or may not be have an accomodative component. Uncorrected hyperopia may result in amblyopia. Cycloplegic refraction followed by optimum refractive correction should be pursued. Apart from vision correction, optical correction may also eliminate some degree of or entire anomalous head posture.74
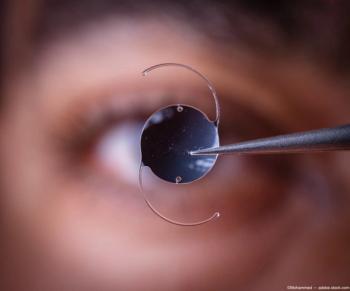
Surgery: Though surgical outcomes are not favorable, surgical interventions are a last resort in the presence of significant head posture and intolerable cosmesis. In general, the surgical plan and aim of strabismus surgery in DRS is usually based on the following:
– Significant deviation in primary position
– Intolerable abnormal head posture
– Severity of globe retraction and overshoots
– Degree of limitation of ductions
– Forced duction testing
– Extent of field of binocular single vision
Optometric vision therapy (OVT): Optometric vision therapy is not a common treatment consideration for patients with DRS, but underlying binocular vision anomalies may cause some of these patients to be symptomatic. A comprehensive binocular and accommodative assessment must be completed before initiating therapy. Well-designed OVT will help in the improvement of binocular functions and overall visual performance.
Conclusion
The current understanding of DRS shows ample forms of clinical presentation whose treatment vary. Current treatment modalities primarily focus on management of head posture and cosmesis and less on binocularity and fixing the ocular restriction. Using OVT, patients with DRS can benefit from symptomatic relief from coexisting ocular morbidities.
References
1. Oystreck DT, Engle EC, Bosley TM. Recent progress in understanding congenital cranial dysinnervation disorders. J Neuroophthalmol. 2011; 31(1):69-77.
2. Duane A. Congenital deficiency of abduction, associated with impairment of adduction, retraction movements, contraction of the palpebral fissure and oblique movements of the eye. Arch Ophthalmol. 1996;114(10):1255-1256.
3. Heuck G. About innate inherited motility defects in the eyes. Klin Monatsbl Augenkeilkd. 1879;17:253.
4. Stilling J, Bergmann JF, editors. Investigations about the emergence of myopia. Germany: Wiesbaden; 1887. p. 13.
5. Turk S. Comments to a case of retraction of the eye. Cbl Pract Augenheilk. 1899;23:14.
6. Bahr K. Vorstellung eines Falles von eigenartiger Muskelanomalie eines Auges. Ber Dtsch Ophthalmol Ges. 1896;25:334.
7. Sinclair WW. Abnormal associated movements of the eyelids. Ophthalmol Rev. 1895;14:307.
8. Wolff J. The occurrence of retraction movements of the eyeball together with congenital defects in the external ocular muscles. Arch Ophthalmol. 1900;29:297.
9. Cook DL. Optometric management of patients with incomitant strabismus. J Behav Optom. 2004;15(1):10-6.
10. DeRespinis PA, Caputo AR, Wagner RS, et al. Duane’s retraction syndrome. Surv Ophthalmol. 1993;38(3):257-288
11. Moster ML. Paresis of isolated and multiple cranial nerves and painful ophthalmoplegia. In: Yanoff M, Duker JS, editors. Ophthalmology. Philadelphia, PA: Mosby; 1999.
12. Kekunnaya R, Gupta A, Sachdeva V, et al. Duane retraction syndrome: series of 441 cases. J Pediatr Ophthalmol Strabismus. 2012;49(3):164-169.
13. Mohan K, Sharma A, Pandav SS. Differences in epidemiological and clinical characteristics between various types of Duane retraction syndrome in 331 patients. J AAPOS. 2008;12(6):576-580.
14. Parsa CF, Robert MP. Thromboembolism and congenital malformations: from Duane syndrome to thalidomide embryopathy. JAMA Ophthalmol. 2013;131(4):439-447.
15. Yüksel D, Orban de Xivry JJ, Lefevre P. Review of the major findings about Duane retraction syndrome (DRS) leading to an updated form of classification. Vision Res. 2010; 50(23): 2334- 2347.
16. Lyle TK, Bridgeman GJO. Worth and Chavasse’s Squint. In: The Binocular Reflexes and the Treatment of Strabismus. 9th ed. London: Bailliere Tindall and Cox, 1959:251-255.
17. Khan AO, Oystreck DT. Clinical characteristics of bilateral Duane syndrome. J AAPOS. 2006;10(3):198-201.
18. Khan AO, Oystreck DT, Wilken K, Akbar F. Duane retraction syndrome on the Arabian peninsula. Strabismus. 2007;15(4):205-208.
19. Apple C. Congenital abducens paralysis. Am J Ophthalmol. 1939;22(2):169.
20. Bielchowsky A. Lectures on motor anomalies of the eyes. Arch Ophthalmol. 1935;13(1):33-59.
21. Duane TD, Schatzz NJ, Caputo AR. Pseudo-Duane retraction syndrome. Trans Am Ophthalmol Soc. 1976;74:122- 32.
22. Scott AB. Upshoot and downshoots. Smith-Kettlewell Symposium on basic sciences in strabismus. V congress of Conselho Latino-Americano de Estrabismo (CLADE) Sao Paulo, Oficinas das Edicoes Loyala, 1978.
23. Souza-Dias C. Additional Consequences of ,uscle co-contraction in Duane’s Syndrome. In symposium on basic sciences in strabismus, Guaruja, Brazil, Oct 16-17, 1976.
24. Gundersen T, Zeavin B. Observations on the retraction syndrome of Duane. Arch Ophthalmol. 1956;55:576.
25. Papst W. [Motility disorders of the eye due to paradoxical innervation]. Klin Monbl Augenheilkd Augenarztl Fortbild. 1962;141:199-209. German.
26. Miller NR, Kiel SM, Green WR, Clark AW. Unilateral Duane’s retraction syndrome (type 1). Arch Ophthalmol. 1982;100(9): 1468-1472.
27. Hotchkiss MG, Miller NR, Clark AW, Green WR. Bilateral Duane’s syndrome. A clinical-pathologic case report. Arch Ophthalmol. 1980;98(5):870-874.
28. Hoyt WF, Nachtigäller H. Anomalies of ocular motor nerves. Neuroanatomic correlates of paradoxical innervation in Duane’s syndrome and related congenital ocular motor disorders. Am J Ophthalmol. 1965;60(3):443-448.
29. Ramsay J, Taylor D. Congenital crocodile tears: a key to the aetiology of Duane’s syndrome. Br J Ophthalmol. 1980;64(7):518-522.
30. Schmidt D. [Congenital eye muscle palsies. Electromyographic and electronystagmographic findings in congenital supranuclear lesions (author’s transl)]. Albrech Von Graefes Arch Klin Exp Ophthalmol. 1974;192(4):285-312.
31. Cullen P, Rodgers CS, Callen DF, et al. Association of familial Duane anomaly and urogenital abnormalities with bisatellited marker derived from chromosome 22. Am J Med Genet. 1993;47(6):925-30.
32. Miyake N, Chilton J, Psatha M, et al. Human CHN1 mutations hyperactivate a2-chimaerin and cause Duane’s retraction syndrome. Science. 2008;321(5890):839-843.
33. Appukuttan B, Gillanders E, Juo SH, et al. Localization of a gene for Duane retraction syndrome to chromosome 2q31. Am J Hum Genet. 1999;65(6):1639-1646.
34. Al-Baradie R, Yamada K, St Hilaire C, et al. Duane radial ray syndrome (Okihiro syndrome) maps to 20q13 and results from mutations in SALL4, a new member of the SAL family. Am J Hum Genet. 2002;71(5):1195-1199.
35. Kohlhase J, Heinrich M, Schubert L, et al. Okihiro syndrome is caused by SALL4 mutations. Hum Mol Genet. 2002;11(23):2979-2987.
36. Mehdorn E, Kommerell G. Inherited Duane’s syndrome. Mirrorlike localization of oculomotor disturbances in monozygotic twins. J Pediatr Ophthalmol Strabismus. 1979;16(3):152-155.
37. Pfaffenbach DD, Cross HE, Kearns TP. Congenital anomalies in Duane’s retraction syndrome. Arch Ophthalmol. 1972;88(6):635-639.
38. Holzmann AE, Chrousos GA, Kozma C, Traboulsi EI. Duane’s retraction syndrome in the fetal alcohol syndrome. Am J Ophthalmol. 1990;110(5):565-6.
39. Hedera P. Friedland RP. Duane syndrome with giant aneurysm of the vertebral basilar arterial junction. J Chin Neuro Ophthalmol. 1993;13(4):271-4.
40. Miller MT, Strömland KK. What can we learn from the thalidomide experience: an ophthalmologic perspective. Curr Opin Ophthalmol. 2011; 22(5):356-64.
41. Gittinger JW Jr, Hughes JP, Suran EL. Medial orbital wall blow-out fracture producing an acquired retraction syndrome. J Clin Neuroophthalmol. 1986;6(3):153-156.
42. Kivlin JD, Lunderman MK. Acquired retraction syndrome associated with orbital metastasis. J Pediatr Ophthalmol Strabismus. 1985; 22(3):109-112.
43. Kargi SH, Atasoy HT, Sayarlioglu H, et al. Acquired retraction of the eye as the first sign of myositis. Strabismus. 2005;13(2):85-88.
44. Sood GC, Srinath BS, Krishnamurthy G. Acquired Duane’s retraction syndrome following Kronlein’s operation. Eye Ear Nose Throat Mon. 1975;54(8):308-310.
45. Khan AO. Inverse globe retraction syndrome complicating recurrent pterygium. Br J Ophthalmol. 2005;89(5):640-641.
46. Yamagami A, Wakakura M, Tsubouchi T, et al. Bilateral Duane’s retraction syndrome due to large pontine glioma. Neuro Ophthalmol Japan. 2003;20(1):66-70.
47. Yüksel D, Orban de Xivry J,J Lefèvre P. Review of the major findings about Duane retraction syndrome (DRS) leading to an updated form of classification. Vision Res. 2010;50(23):2334- 2347.
48. Silverberg M, Demer J. Duane’s syndrome with compressive denervation of the lateral rectus muscle. Am J Ophthalmol. 2001;131(1): 146-148.
49. Smith JL, Damast M. Acquired retraction syndrome after sixth nerve palsy. Br J Ophthalmol. 1973;57(2):110-114.
50. Gaur N, Sharma P. Management of Duane retraction syndrome: A simplified approach. Indian J Ophthalmol. 2019; 67:16-22.
51. Malbran J. Estrabismos y paralysis. Clinica y terapeutua. Editorial Oftalmologia. 1949;625.
52. Papst W. Paralytischer Strabismus infolge paradoxer innervation. Ber Zusammenkunft Dtsch Ophthalmol Ges. 1966;67:84-101.
53. Brown HW. Congenital structural muscle anomalies. In: Allen JH, ed. Strabismus Ophthalmic Symposium. St Louis: Mosby. 1950;205-36.
54. Huber A. Electrophysiology of the retraction syndromes. Br J Ophthalmol. 1974;58(3):293-300.
55. Ravindran M, Pawar N, Karkera RP, Kunnatur R. Clinical analysis, management and outcome of Duane’s retraction syndrome at a Tertiary Eye Care Centre in South India. Delhi Ophthalmol Soc. 2013; 24:97-101.
56. von Noorden GK. Binocular vision and ocular motility: theory and management of strabismus. 5th ed. St. Louis: Mosby, 1996:430-7.
57. Kirkham TH. Anisometropia and amblyopia in Duane’s syndrome. Am J Ophthalmol. 1970;69:774-777.
58. Ahluwalia BK, Gupta NC, Goel SR, Khurana AK. Study of Duane’s retraction syndrome. Acta Ophthalmologica. 1988;66(6):728-730.
59. Kirkham TH. Inheritance of Duane’s syndrome. Br J Ophthalmol. 1970; 54(5):323-329.
60. O’Malley ER, Helveston EM, Ellis FD. Duane’s retraction syndromeplus. J Pediatr Ophthalmol Strabismus. 1982;19(3):161- 165.
61. Isenberg S, Urist MJ. Clinical observations in 101 consecutive patients with Duane’s retraction syndrome. Am J Ophthalmol. 1977;84(3):419-425.
62. Hering E. In: Die Lehre vom Binoculren Sehen. Leipzig, Germany: Wilhelm Englemann; 1868.
63. Chung M, Stout JT, Borchert MS. Clinical diversity of hereditary Duane’s retraction syndrome. Ophthalmology. 2000;107(3):500-503.
64. Kekunnaya R, Moharana R, Tibrewal S, Chhablani PP, Sachdeva V. A simple and novel grading method for retraction and overshoot in Duane retraction syndrome. Br J Ophthalmol. 2016;100(11):1451-1454.
65. Wildervanck LS. A case of Klippel-Feil’s syndrome with abducens paralysis; retraction of the eyeball and deaf-mutism. Ned Tijdschr Geneeskd. 1952;96(44):2752–2756.
66. Wilcox LM, Gittinger JW, Breinin GM. Congenital adduction palsy and synergistic divergence. Am J Ophthalmol. 1981;91(1):1-7.
67. Collins ET. Enophthalmos. Br Med J. 1899;2:846-851.
68. Cibis GW. Congenital familial external ophthalmoplegia with co-contraction. Ophthalmic Paediatr Genetics. 1984;4(3):163- 167.
69. Weiss IS, Urist MJ. Duane’s syndrome associated with tendon sheath syndrome and microcornea. J Pediatr Ophthalmol Strabismus. 1972;9(1):14-15.
70. Graeber CP, Hunter DG, Engle EC. The genetic basis of incomitant strabismus: consolidation of the current knowledge of the genetic foundations of disease. Semin Ophthalmol. 2013;28(5-6):427-437
71. Yang MM, Ho M, Lau HH, et al. Diversified clinical presentations associated with a novel sal-like 4 gene mutation in a Chinese pedigree with Duane retraction syndrome. Mol Vis. 2013;19:986-994.
72. Griffin JR, Carlson GP. Duane Retraction Syndrome and vision therapy: A case report. J Am Optom Assoc. 1991;62(4):318-21.
73. Jampolsky AJ. Duane syndrome. In: Rosenbaum AL, Santiago AP, eds. Clinical strabismus management: principles and surgical techniques. Philadelphia: WB Saunders, 1999:325- 46.
74. Kekunnaya R, Velez FG, Pineles SL. Outcomes in patients with esotropic duane retraction syndrome and a partially accommodative component. Indian J Ophthalmol. 2013;61(12):701-704.
Articles in this issue
almost 5 years ago
Quiz: Patient experiences sudden decrease in visionalmost 5 years ago
Soft toric lens fitting practices not meeting patient needsalmost 5 years ago
Point-of-care testing helps dry eye diagnosisalmost 5 years ago
Patient experiences sudden decrease in visionalmost 5 years ago
How to improve telehealthalmost 5 years ago
High IOP, uveitis lead to Posner-Schlossman diagnosisalmost 5 years ago
Differential key to diagnosing idiopathic orbital inflammationabout 5 years ago
How to avoid patient nonadherenceNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.