- Optometry Times Vol. 10 No. 11
- Volume 10
- Issue 11
How hyperopes differ from myopes
My mother’s prescription was +6.00-3.00 x 178 or so in each eye prior to cataract surgery; my 20-year-old daughter’s prescription is +5.75-2.50x07. Aren’t genetics grand?
Both started wearing glasses around the age of 4, with my daughter’s refractive error confirmed when we first installed a WaveScan WaveFront System (VisX/AMO) at the laser center.
When I say hyperopes are “different,” I say it with love and affection as well as with professional knowledge. Let’s discuss the “how” and “why” of hyperopes being different and what their options are for refractive procedures.
Explaining hyperopes
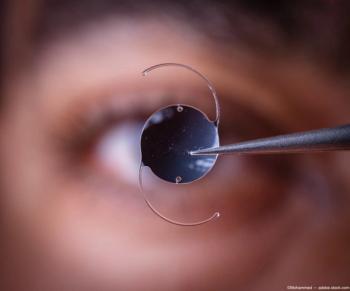
When a patient’s hyperopia gets above +2.00 D or so, ODs need to think about how it will affect the patient’s glasses and/or contact lenses. We all know a plus lens is thicker in the center and thinner in the periphery.
Proper frame selection and ophthalmic lens materials have become important to achieve acceptable cosmesis.
Why is it that a +6.00 D hyperope is attracted to the largest frame on an OD’s board?
Similarly, contact lenses are thicker in the center. So a hyperope’s contact lens is harder to handle and harder to apply and transmits less oxygen to the cornea.
Additionally, without correction, many hyperopes cannot see their fingers clearly to apply the lens and need some type of correction just to start the process.
Examining the literature
Hyperopes are different in other ways as well. Results from a vocational interest survey study of 140 male students found that 76 percent reported a likelihood of predicting myopia versus hyperopia. Hyperopes were more interested in business skills and selling but also less likely to become officers.1
Another study of 152 military recruits found hyperopes to significantly vary from myopes in weight and heart rate variability. Hyperopes weighed more and had a lower heart rate variability (HRV).2 A low heart has been associated with a poorer ability to adapt to stress. The Framingham Heart Study found poorer cardiovascular function in patients with low HRV.3-4
Finally, a study of 782 incoming students at Washington State University-which included females-found certain personality differences, with hyperopes more extroverted than myopes. Hyperopes are different.5
Laser vision correction
Hyperopes are also different as it relates to laser vision correction. As lasers improve, the first U.S. Food & Drug Administration (FDA) approvals are almost always for myopes.6
This is partly because the market is much larger but also because the treatment is different. A hyperopic treatment removes tissue in the mid-periphery that can blend out to 9 mm, making the cornea relatively steeper and increasing the power of the cornea.
Hyperopic treatments are typically longer and, with early lasers, could take up to one minute of lasering time. Such lengths lead to varying treatments and varying healing with the result and poorer outcomes as measured by patients achieving uncorrected vision of 20/20.7
Hyperopic treatments differ from myopic treatments both optically and physiologically. Hyperopic treatments result in a more prolate cornea while also having a smaller effective optic zone.8
These treatments have a larger angle kappa, and this emphasizes the importance of properly centering the treatment.9
Then comes the debate of where to center the treatment: pupil center, corneal apex, visual axis or somewhere in between.
Studies trend toward centering the treatment over the visual axis.10,11 Critical to centering the treatment is having a laser that can track the cornea accurately.12
Ocular surface
The treatment for hyperopic patients takes place in the mid-periphery blending out to the periphery. This damages more corneal nerves and results in patients having more challenges with their ocular surfaces after procedures.13
It is also important that ODs carefully examine hyperopic patient pre-operatively for ocular surface disease and meibomian gland dysfunction. Also, look for concomitant risk factors for dry eye such as gender, age, smoking, and medications.
Addressing and treating the condition prior to surgery can be more effective than trying to play “catch-up” after surgery. Treatments can include artificial tears, prescription medicines such as lifitegrast (Xiidra, Shire) and/or cyclosporine (Restasis, Allergan; Cequa, Sun Pharma), lid scrubs and meibomian gland treatments such as iLux (Tear Film Innovations) or LipiFlow (Johnson & Johnson Vision). Treatments can continue after surgery.
Results
Long-term results for hyperopic treatments appear less stable than those of myopic patients.14 There are two proposed mechanisms for the regression that is seen with hyperopic treatments:
First is latent hyperopia not detected pre-operatively. Therefore, it is important to obtain an accurate cycloplegic refraction, typically using cyclopentolate (Cyclogyl, Alcon). If there is a significant difference in sphere power between the manifest refraction and the cycloplegic refraction, delaying or postponing surgery is an option to consider.
Often when the full cycloplegic refraction is treated, post-operatively the eye tries to maintain its altered accommodative state, resulting in post-operative pseudo-myopia.
Secondly, hyperopic treatments can show a progressive change in the corneal curvature and decrease in corneal power. Studies have look at causes for this increase in regression.
A 2005 study concluded, “Less predictable biomechanical changes from the circumferential release of tension on collagen bundles after midperipheral hyperopic ablation and greater variation in beam centration and the angle of incidence may contribute to the greater variability in corneal curvature and power in hyperopic LASIK than in myopic LASIK.”15
This points to a biomechanical difference. Other studies point toward epithelial changes creating a relative flattening of the cornea.16
The paracentral epithelium has been shown to thicken post-operatively, reducing the effect of the treatment. The greater the treatment in SE hyperopia, the more aggressive the epithelial remodeling.17 The greater the treatment, the greater the trough that needs to be filled. Epithelium does what it needs to and fills the trough.
Research has also identified micro fibroblast proliferation leading to stromal remodeling in hyperopic treatments.18 One study showed regression over the first five years post-surgery and limited regression up to 16 years after.19
Current methods
Today, the excimer laser operates at a much higher rate than in years ago, and treatment times for hyperopes are as short as ever. Ablation patterns continue to evolve to limit regression and maintain optical quality.
Methods to modulate and measure epithelium proliferation are in development, which have shown more stable hyperopic treatments.20 Nevertheless, it is important to remember hyperopes are different.
Today, the excimer laser operates at a much higher rate than in years ago, and treatment times for hyperopes are as short as ever. Ablation patterns continue to evolve to limit regression and maintain optical quality.
Methods to modulate and measure epithelium proliferation are in development, which have shown more stable hyperopic treatments.20 Nevertheless, it is important to remember hyperopes are different.
References:
1. Young FA, Singer RM, Foster D. The psychological differentiation of male myopes and nonmyopes. Am J Optom Physiol Opt. 1975 Oct;52(10):679-86.
2. Gawron VJ. Differences among myopes, emmetropes, and hyperopes. Am J Optom Physiol Opt. 1981 Sep;58(9):753-60.
3. Buccelletti E, Gilardi E, Scaini E, Galiuto L, Persiani R, Biondi A, Basile F, Silveri NG. Heart rate variability and myocardial infarction: systematic literature review and metanalysis. Eur Rev for Med Pharmacol Sci. 2009 Jul-Aug;13(4):299-307.
4. Tsuji H, Venditti FJ Jr, Manders ES, Evans JC, Larson MG, Feldman CL, Levy D. Reduced heart rate variability and mortality risk in an elderly cohort. The Framingham Heart Study. Circulation,1994 Aug;90(2):878-83.
5. Beedle SL, Young FA. Values, personality, physical characteristics, and refractive error. Am J Optom Physiol Opt. 1976 Nov;53(11):735-9.
6. U.S. Food and Drug Administration. List of FDA-Approved Lasers for LASIK. U.S. Department of Health and Human Services. Available at: https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/SurgeryandLifeSupport/LASIK/ucm192109.htm. Accessed on 10/29/18.
7. Kohnen T, Mohoumud K. Comparison of corneal higher-order aberrations induced by myopic and hyperopic LASIK; Ophthalmology. 2005 Oct;112(10):1692.
8. Zadok D, Raifkup F, Landau D, Frucht-Pery J. Long-term evaluation of hyperopic laser in situ keratomileusis. J Cataract Refract Surg. 2003 Nov;29:2181–2188.
9. Basmak H, Sahin A, Yildirim N, Papakostas TD, Kanellopoulos AJ. Measurement of angle kappa with synoptophore and Orbscan II in a normal population. J Refract Surg. 2007 May;23:456–60.
10. Nepomuceno RL, Boxer BS, Wachler, Kim JM, Scruggs R, Sato M. Laser in situ keratomileusis for hyperopia with the LADARVision 4000 with centration on the coaxially sighted corneal light reflex. J Cataract Refract Surg. 2004 Jun;30:1281-6.
11. Wachler BS, Korn TS, Chandra NS, Michel FK. Decentration of the optical zone: centering on the pupil versus the coaxially sighted corneal light reflex in LASIK for hyperopia. J Refract Surg. 2003 Jul-Aug;19:464-5.
12. Kermani O. Alignment in customized laser in situ keratomileusis. J Refract Surg. 2004 Sep-Oct;20(5 Suppl):S651–8.
13. Esquenazi S. Five-year follow-up of laser in situ keratomileusis for hyperopia using the Technolas Keracor 117C excimer laser. J Refract Surg. 2004 Jul-Aug;20(4):356-63.
14. A. B. Plaza-Puche, P. Yebana, S. Arba-Mosquera, and J. L. Alió. Three-year follow-up of hyperopic LASIK using a 500-Hz excimer laser system. J Refract Surg. 2015 Oct;31(10):674-82.
15. Qazi MA, Roberts CJ, Mahmoud AM, Pepose JS. Topographic and biomechanical differences between hyperopic and myopic laser in situ keratomileusis. J Cataract Refract Surg. 2005 Jan;31(1):48-60.
16.Reinstein DZ, Carp GI, Archer TJ, Buick T, Gobbe M, Rowe EL, Jukic M, Brandon E, Moore J, Moore T. LASIK for the Correction of High Hyperopic Astigmatism With Epithelial Thickness Monitoring. J Refract Surg. 2017 May 1;33(5):314-321.
17. Wilson SE, Kim WJ. Keratocyte apoptosis: implications on corneal wound healing, tissue organization, and disease. Invest Ophthalmol Vis Sci. 1998 Feb;39(2):220-6.
18. Alio JL, Gharaibeh A, Mas D, Espinosa J, Villanueva A. Corneal stability following LASIK for hyperopic correction: objective analysis by a light propagation algorithm. 2018 Mar: 1-10.
19. Dave R, O'Brart DP, Wagh VK, Lim WS, Patel P, Lee J, Marshall J. Sixteen-year follow-up of hyperopic laser in situ keratomileusis. J Cataract Refract Surg. 2016 May;42(5):717-24. doi: 10.1016/j.jcrs.2016.03.028.
20. Reinstein DZ, Carp GI, Archer TJ, Buick T, Gobbe M, Rowe EL, Jukic M, Brandon E, Moore J, Moore T. LASIK for the correction of high hyperopic astigmatism with epithelial thickness monitoring. J Refract Surg. 2017 May 1;33(5):314-321.
Articles in this issue
about 7 years ago
How to handle non-ophthalmic emergenciesabout 7 years ago
Q&A: Cornea, almost two residencies, and a Vietnamese hoagieabout 7 years ago
Imaging aids in differential diagnosis of uncommon diseaseabout 7 years ago
Why doctors are rethinking AMD standardsover 7 years ago
Know the link between cotton wool spot and anemiaover 7 years ago
Knowing when to delegate testing responsibilitiesover 7 years ago
When to refer patients with diabetic retinopathyover 7 years ago
Dialogue with lecturers at CEover 7 years ago
5 steps to manage cataract patient expectationsNewsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.