Diabetic Eye Disease
Latest News
CME Content







Non-eyecare practitioners will be screening your patients for diabetic retinopathy. Find out why this can help or hurt your patients and how you can help guide the process.

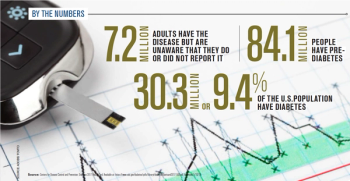
More than 9 percent of U.S. adults have diabetes, and those patients are sitting in your chair. Find out how diabetes affects your patients’ vision.

Patients with diabetes may need to add a dry eye workup to their health assessments. Scott Schwartz, OD, from Detroit, MI, discusses his poster, “Does diabetes make a difference in dry eye,” at ARVO 2018 in Honolulu.


ODs may wish to incorporate color vision testing when working with patients having diabetes. A. Paul Chous, MA, OD, FAAO, CDE, talks about the importance of these tests, incorporating them into day-to-day exams, and devices available.

Diagnosing and treating diabetic macular edema (DME) can pose a challenge for ODs. A. Paul Chous, OD, MA, FAAO, CDE, examines a case of non-center involved DME and the challenges he faced when treating one patient.

It is important for eyecare providers to be familiar with these new drugs and findings. We often see patients with diabetes, metabolic syndrome, and high CV risk, and we are in a position to help counsel our patients about new treatments-and even suggest that appropriate patients have conversations with their primary-care physicians, endocrinologists and cardiologists.

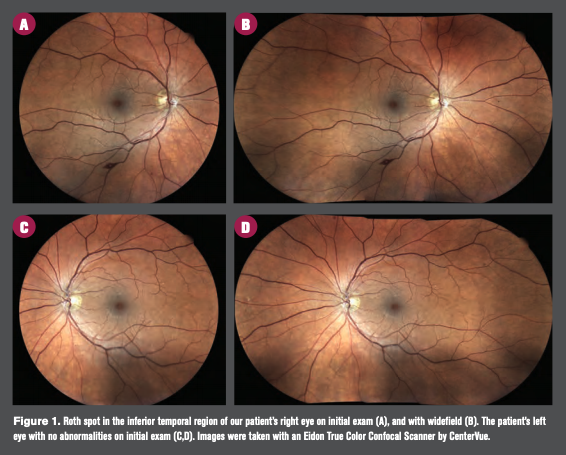
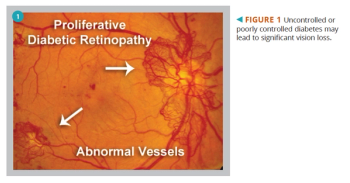
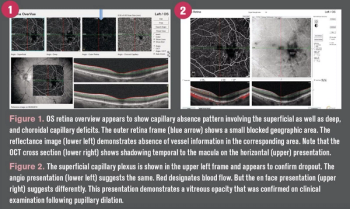
A 30-year-old female with a 16-year history of insulin-dependent diabetes and no other ocular or systemic conditions developed proliferative retinopathy in March 2015. She had not been closely followed for the previous five years.

Recognize characteristics and stages of macular hole for better pictures

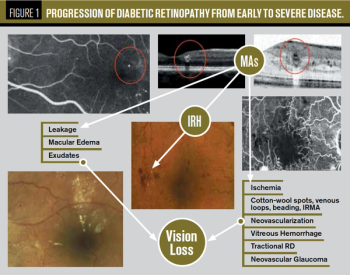
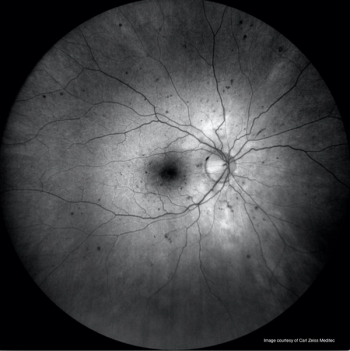
Diabetic retinopathy (DR) in patients is a common finding in optometric practices. When we grade the level of retinopathy, we often do so with findings of the Early Treatment Diabetic Retinopathy Study (ETDRS)in mind.

Let’s examine case-based examples to emphasize the top five neuro-ophthalmic disorders that should not be overlooked.

A colleague recently told me that eye doctors should “stay within the lines” of traditional eye care because we barely have enough time as it is to do our jobs. My response was that today more than half of our adult patients have either diabetes or prediabetes, so our job now requires we go ”outside the lines” to avoid the leading cause of preventable blindness.

Given this abundance of nonhuman species living on and within our bodies, it is not surprising that there is a link between specific bacteria to systemic and ocular disease-including diabetes and diabetes-related eye disease.